npj Regenerative Medicine ( IF 6.4 ) Pub Date : 2018-01-31 , DOI: 10.1038/s41536-017-0038-8 M Mirazul Islam 1, 2 , Oleksiy Buznyk 1, 3 , Jagadesh C Reddy 4 , Nataliya Pasyechnikova 3 , Emilio I Alarcon 5 , Sally Hayes 6, 7 , Philip Lewis 6, 7 , Per Fagerholm 1 , Chaoliang He 8 , Stanislav Iakymenko 3 , Wenguang Liu 9 , Keith M Meek 6, 7 , Virender S Sangwan 4 , May Griffith 1, 4, 10
|
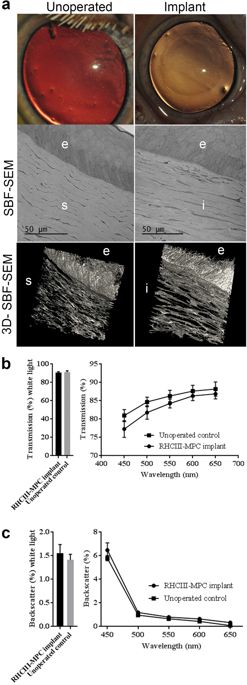
The severe worldwide shortage of donor organs, and severe pathologies placing patients at high risk for rejecting conventional cornea transplantation, have left many corneal blind patients untreated. Following successful pre-clinical evaluation in mini-pigs, we tested a biomaterials-enabled pro-regeneration strategy to restore corneal integrity in an open-label observational study of six patients. Cell-free corneal implants comprising recombinant human collagen and phosphorylcholine were grafted by anterior lamellar keratoplasty into corneas of unilaterally blind patients diagnosed at high-risk for rejecting donor allografts. They were followed-up for a mean of 24 months. Patients with acute disease (ulceration) were relieved of pain and discomfort within 1–2 weeks post-operation. Patients with scarred or ulcerated corneas from severe infection showed better vision improvement, followed by corneas with burns. Corneas with immune or degenerative conditions transplanted for symptom relief only showed no vision improvement overall. However, grafting promoted nerve regeneration as observed by improved touch sensitivity to near normal levels in all patients tested, even for those with little/no sensitivity before treatment. Overall, three out of six patients showed significant vision improvement. Others were sufficiently stabilized to allow follow-on surgery to restore vision. Grafting outcomes in mini-pig corneas were superior to those in human subjects, emphasizing that animal models are only predictive for patients with non-severely pathological corneas; however, for establishing parameters such as stable corneal tissue and nerve regeneration, our pig model is satisfactory. While further testing is merited, we have nevertheless shown that cell-free implants are potentially safe, efficacious options for treating high-risk patients.
中文翻译:

生物材料使供体组织移植排斥反应高风险患者的角膜再生
世界范围内供体器官的严重短缺,以及使患者面临拒绝常规角膜移植的高风险的严重病理,使许多角膜盲患者得不到治疗。在对小型猪进行成功的临床前评估后,我们在对六名患者的开放标签观察研究中测试了一种支持生物材料的促再生策略,以恢复角膜完整性。包含重组人胶原蛋白和磷酸胆碱的无细胞角膜植入物通过前板层角膜移植术移植到被诊断为排斥供体同种异体移植物高风险的单侧失明患者的角膜中。他们的平均随访时间为 24 个月。急性疾病(溃疡)患者在术后 1-2 周内减轻疼痛和不适。严重感染导致角膜瘢痕或溃疡的患者视力改善较好,其次是烧伤角膜。为缓解症状而移植的具有免疫或退化性疾病的角膜仅显示整体视力没有改善。然而,移植促进了神经再生,正如所有测试患者的触摸敏感性提高到接近正常水平所观察到的那样,即使对于那些在治疗前几乎没有/没有敏感性的患者也是如此。总体而言,六分之三的患者视力显着改善。其他人则足够稳定,可以进行后续手术以恢复视力。小型猪角膜的移植结果优于人类受试者,强调动物模型仅可预测患有非严重病理性角膜的患者;然而,对于建立稳定的角膜组织和神经再生等参数,我们的猪模型是令人满意的。虽然值得进一步测试,但我们仍然表明,无细胞植入物是治疗高危患者的潜在安全、有效的选择。











































 京公网安备 11010802027423号
京公网安备 11010802027423号