Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Association of Insulin Pump Therapy vs Insulin Injection Therapy With Severe Hypoglycemia, Ketoacidosis, and Glycemic Control Among Children, Adolescents, and Young Adults With Type 1 Diabetes
JAMA ( IF 63.1 ) Pub Date : 2017-10-10 , DOI: 10.1001/jama.2017.13994 Beate Karges 1 , Anke Schwandt 2, 3 , Bettina Heidtmann 4 , Olga Kordonouri 5 , Elisabeth Binder 6 , Ulrike Schierloh 7 , Claudia Boettcher 8 , Thomas Kapellen 9 , Joachim Rosenbauer 3, 10 , Reinhard W. Holl 2, 3
JAMA ( IF 63.1 ) Pub Date : 2017-10-10 , DOI: 10.1001/jama.2017.13994 Beate Karges 1 , Anke Schwandt 2, 3 , Bettina Heidtmann 4 , Olga Kordonouri 5 , Elisabeth Binder 6 , Ulrike Schierloh 7 , Claudia Boettcher 8 , Thomas Kapellen 9 , Joachim Rosenbauer 3, 10 , Reinhard W. Holl 2, 3
Affiliation
|
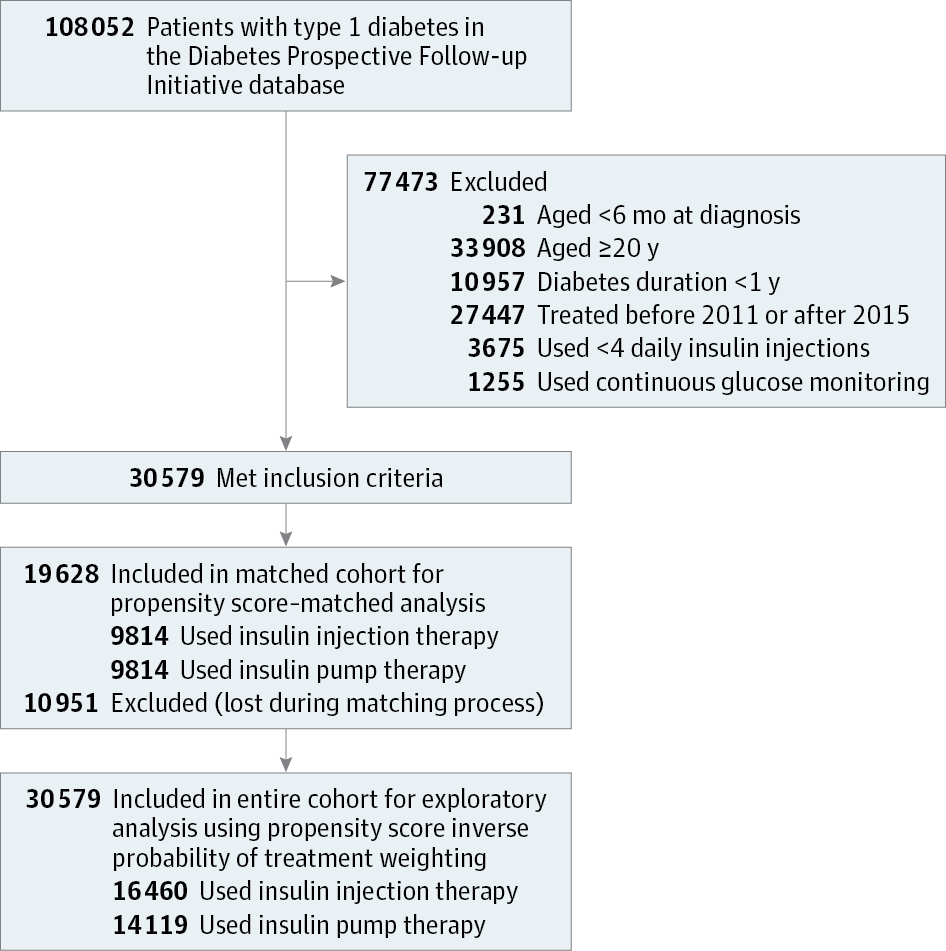
Importance Insulin pump therapy may improve metabolic control in young patients with type 1 diabetes, but the association with short-term diabetes complications is unclear. Objective To determine whether rates of severe hypoglycemia and diabetic ketoacidosis are lower with insulin pump therapy compared with insulin injection therapy in children, adolescents, and young adults with type 1 diabetes. Design, Setting, and Participants Population-based cohort study conducted between January 2011 and December 2015 in 446 diabetes centers participating in the Diabetes Prospective Follow-up Initiative in Germany, Austria, and Luxembourg. Patients with type 1 diabetes younger than 20 years and diabetes duration of more than 1 year were identified. Propensity score matching and inverse probability of treatment weighting analyses with age, sex, diabetes duration, migration background (defined as place of birth outside of Germany or Austria), body mass index, and glycated hemoglobin as covariates were used to account for relevant confounders. Exposures Type 1 diabetes treated with insulin pump therapy or with multiple (≥4) daily insulin injections. Main Outcomes and Measures Primary outcomes were rates of severe hypoglycemia and diabetic ketoacidosis during the most recent treatment year. Secondary outcomes included glycated hemoglobin levels, insulin dose, and body mass index. Results Of 30 579 patients (mean age, 14.1 years [SD, 4.0]; 53% male), 14 119 used pump therapy (median duration, 3.7 years) and 16 460 used insulin injections (median duration, 3.6 years). Patients using pump therapy (n = 9814) were matched with 9814 patients using injection therapy. Pump therapy, compared with injection therapy, was associated with lower rates of severe hypoglycemia (9.55 vs 13.97 per 100 patient-years; difference, −4.42 [95% CI, −6.15 to −2.69]; P < .001) and diabetic ketoacidosis (3.64 vs 4.26 per 100 patient-years; difference, −0.63 [95% CI, −1.24 to −0.02]; P = .04). Glycated hemoglobin levels were lower with pump therapy than with injection therapy (8.04% vs 8.22%; difference, −0.18 [95% CI, −0.22 to −0.13], P < .001). Total daily insulin doses were lower for pump therapy compared with injection therapy (0.84 U/kg vs 0.98 U/kg; difference, −0.14 [−0.15 to −0.13], P < .001). There was no significant difference in body mass index between both treatment regimens. Similar results were obtained after propensity score inverse probability of treatment weighting analyses in the entire cohort. Conclusions and Relevance Among young patients with type 1 diabetes, insulin pump therapy, compared with insulin injection therapy, was associated with lower risks of severe hypoglycemia and diabetic ketoacidosis and with better glycemic control during the most recent year of therapy. These findings provide evidence for improved clinical outcomes associated with insulin pump therapy compared with injection therapy in children, adolescents, and young adults with type 1 diabetes.
中文翻译:

在患有 1 型糖尿病的儿童、青少年和年轻成人中,胰岛素泵疗法与胰岛素注射疗法与严重低血糖、酮症酸中毒和血糖控制的关联
重要性 胰岛素泵治疗可能会改善年轻 1 型糖尿病患者的代谢控制,但与短期糖尿病并发症的关联尚不清楚。目的 确定与胰岛素注射疗法相比,在患有 1 型糖尿病的儿童、青少年和年轻成人中,胰岛素泵疗法的严重低血糖和糖尿病酮症酸中毒的发生率是否更低。设计、设置和参与者 基于人群的队列研究于 2011 年 1 月至 2015 年 12 月在德国、奥地利和卢森堡参与糖尿病前瞻性随访计划的 446 家糖尿病中心进行。确定了年龄小于 20 岁且糖尿病病程超过 1 年的 1 型糖尿病患者。倾向评分匹配和逆概率治疗加权分析与年龄、性别、糖尿病病程、移民背景(定义为出生地在德国或奥地利以外)、体重指数和糖化血红蛋白作为协变量用于解释相关混杂因素。暴露 使用胰岛素泵疗法或每天多次 (≥4) 注射胰岛素治疗的 1 型糖尿病。主要结果和措施主要结果是最近治疗年度中严重低血糖和糖尿病酮症酸中毒的发生率。次要结果包括糖化血红蛋白水平、胰岛素剂量和体重指数。结果 在 30 579 名患者(平均年龄,14.1 岁 [SD,4.0];53% 男性)中,14 119 名使用泵疗法(中位持续时间,3.7 年)和 16 460 次使用胰岛素注射(中位持续时间,3.6 年)。使用泵疗法的患者 (n = 9814) 与使用注射疗法的 9814 名患者相匹配。泵疗法,与注射疗法相比,与较低的严重低血糖发生率相关(每 100 患者年 9.55 比 13.97;差异,-4.42 [95% CI,-6.15 至 -2.69];P < .001)和糖尿病酮症酸中毒(3.64 比每 100 患者年 4.26;差异,-0.63 [95% CI,-1.24 至 -0.02];P = .04)。泵疗法的糖化血红蛋白水平低于注射疗法(8.04% 与 8.22%;差异,-0.18 [95% CI,-0.22 至 -0.13],P < .001)。与注射疗法相比,泵疗法的每日总胰岛素剂量较低(0.84 U/kg vs 0.98 U/kg;差异,-0.14 [-0.15 至 -0.13],P < .001)。两种治疗方案之间的体重指数没有显着差异。在整个队列中进行治疗加权分析的倾向评分逆概率后获得了类似的结果。结论和相关性 在年轻的 1 型糖尿病患者中,与胰岛素注射治疗相比,胰岛素泵治疗与最近一年治疗期间发生严重低血糖和糖尿病酮症酸中毒的风险较低以及更好的血糖控制相关。这些发现为儿童、青少年和年轻成人 1 型糖尿病患者的胰岛素泵治疗与注射治疗相比改善了临床结果提供了证据。
更新日期:2017-10-10
中文翻译:

在患有 1 型糖尿病的儿童、青少年和年轻成人中,胰岛素泵疗法与胰岛素注射疗法与严重低血糖、酮症酸中毒和血糖控制的关联
重要性 胰岛素泵治疗可能会改善年轻 1 型糖尿病患者的代谢控制,但与短期糖尿病并发症的关联尚不清楚。目的 确定与胰岛素注射疗法相比,在患有 1 型糖尿病的儿童、青少年和年轻成人中,胰岛素泵疗法的严重低血糖和糖尿病酮症酸中毒的发生率是否更低。设计、设置和参与者 基于人群的队列研究于 2011 年 1 月至 2015 年 12 月在德国、奥地利和卢森堡参与糖尿病前瞻性随访计划的 446 家糖尿病中心进行。确定了年龄小于 20 岁且糖尿病病程超过 1 年的 1 型糖尿病患者。倾向评分匹配和逆概率治疗加权分析与年龄、性别、糖尿病病程、移民背景(定义为出生地在德国或奥地利以外)、体重指数和糖化血红蛋白作为协变量用于解释相关混杂因素。暴露 使用胰岛素泵疗法或每天多次 (≥4) 注射胰岛素治疗的 1 型糖尿病。主要结果和措施主要结果是最近治疗年度中严重低血糖和糖尿病酮症酸中毒的发生率。次要结果包括糖化血红蛋白水平、胰岛素剂量和体重指数。结果 在 30 579 名患者(平均年龄,14.1 岁 [SD,4.0];53% 男性)中,14 119 名使用泵疗法(中位持续时间,3.7 年)和 16 460 次使用胰岛素注射(中位持续时间,3.6 年)。使用泵疗法的患者 (n = 9814) 与使用注射疗法的 9814 名患者相匹配。泵疗法,与注射疗法相比,与较低的严重低血糖发生率相关(每 100 患者年 9.55 比 13.97;差异,-4.42 [95% CI,-6.15 至 -2.69];P < .001)和糖尿病酮症酸中毒(3.64 比每 100 患者年 4.26;差异,-0.63 [95% CI,-1.24 至 -0.02];P = .04)。泵疗法的糖化血红蛋白水平低于注射疗法(8.04% 与 8.22%;差异,-0.18 [95% CI,-0.22 至 -0.13],P < .001)。与注射疗法相比,泵疗法的每日总胰岛素剂量较低(0.84 U/kg vs 0.98 U/kg;差异,-0.14 [-0.15 至 -0.13],P < .001)。两种治疗方案之间的体重指数没有显着差异。在整个队列中进行治疗加权分析的倾向评分逆概率后获得了类似的结果。结论和相关性 在年轻的 1 型糖尿病患者中,与胰岛素注射治疗相比,胰岛素泵治疗与最近一年治疗期间发生严重低血糖和糖尿病酮症酸中毒的风险较低以及更好的血糖控制相关。这些发现为儿童、青少年和年轻成人 1 型糖尿病患者的胰岛素泵治疗与注射治疗相比改善了临床结果提供了证据。











































 京公网安备 11010802027423号
京公网安备 11010802027423号