Journal of Hepatology ( IF 26.8 ) Pub Date : 2022-09-22 , DOI: 10.1016/j.jhep.2022.09.012 Jiří Reiniš 1 , Oleksandr Petrenko 2 , Benedikt Simbrunner 2 , Benedikt S Hofer 2 , Filippo Schepis 3 , Marco Scoppettuolo 3 , Dario Saltini 3 , Federica Indulti 3 , Tomas Guasconi 3 , Agustin Albillos 4 , Luis Téllez 4 , Càndid Villanueva 5 , Anna Brujats 5 , Juan Carlos Garcia-Pagan 6 , Valeria Perez-Campuzano 6 , Virginia Hernández-Gea 6 , Pierre-Emmanuel Rautou 7 , Lucile Moga 7 , Thomas Vanwolleghem 8 , Wilhelmus J Kwanten 8 , Sven Francque 8 , Jonel Trebicka 9 , Wenyi Gu 10 , Philip G Ferstl 10 , Lise Lotte Gluud 11 , Flemming Bendtsen 11 , Søren Møller 12 , Stefan Kubicek 1 , Mattias Mandorfer 13 , Thomas Reiberger 2
|
Background & Aims
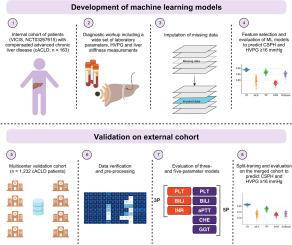
In individuals with compensated advanced chronic liver disease (cACLD), the severity of portal hypertension (PH) determines the risk of decompensation. Invasive measurement of the hepatic venous pressure gradient (HVPG) is the diagnostic gold standard for PH. We evaluated the utility of machine learning models (MLMs) based on standard laboratory parameters to predict the severity of PH in individuals with cACLD.
Methods
A detailed laboratory workup of individuals with cACLD recruited from the Vienna cohort (NCT03267615) was utilised to predict clinically significant portal hypertension (CSPH, i.e., HVPG ≥10 mmHg) and severe PH (i.e., HVPG ≥16 mmHg). The MLMs were then evaluated in individual external datasets and optimised in the merged cohort.
Results
Among 1,232 participants with cACLD, the prevalence of CSPH/severe PH was similar in the Vienna (n = 163, 67.4%/35.0%) and validation (n = 1,069, 70.3%/34.7%) cohorts. The MLMs were based on 3 (3P: platelet count, bilirubin, international normalised ratio) or 5 (5P: +cholinesterase, +gamma-glutamyl transferase, +activated partial thromboplastin time replacing international normalised ratio) laboratory parameters. The MLMs performed robustly in the Vienna cohort. 5P-MLM had the best AUCs for CSPH (0.813) and severe PH (0.887) and compared favourably to liver stiffness measurement (AUC: 0.808). Their performance in external validation datasets was heterogeneous (AUCs: 0.589-0.887). Training on the merged cohort optimised model performance for CSPH (AUCs for 3P and 5P: 0.775 and 0.789, respectively) and severe PH (0.737 and 0.828, respectively).
Conclusions
Internally trained MLMs reliably predicted PH severity in the Vienna cACLD cohort but exhibited heterogeneous results on external validation. The proposed 3P/5P online tool can reliably identify individuals with CSPH or severe PH, who are thus at risk of hepatic decompensation.
Impact and implications
We used machine learning models based on widely available laboratory parameters to develop a non-invasive model to predict the severity of portal hypertension in individuals with compensated cirrhosis, who currently require invasive measurement of hepatic venous pressure gradient. We validated our findings in a large multicentre cohort of individuals with advanced chronic liver disease (cACLD) of any cause. Finally, we provide a readily available online calculator, based on 3 (platelet count, bilirubin, international normalised ratio) or 5 (platelet count, bilirubin, activated partial thromboplastin time, gamma-glutamyltransferase, choline-esterase) widely available laboratory parameters, that clinicians can use to predict the likelihood of their patients with cACLD having clinically significant or severe portal hypertension.
中文翻译:

使用机器学习模型评估代偿性肝硬化患者门脉高压的严重程度
背景与目标
在患有代偿性晚期慢性肝病 (cACLD) 的个体中,门脉高压 (PH) 的严重程度决定了失代偿的风险。肝静脉压力梯度 (HVPG) 的侵入性测量是诊断 PH 的金标准。我们根据标准实验室参数评估了机器学习模型 (MLM) 预测 cACLD 患者 PH 严重程度的效用。
方法
对从维也纳队列(NCT03267615)招募的 cACLD 个体进行详细的实验室检查,用于预测临床显着的门静脉高压(CSPH,即HVPG ≥10 mmHg)和严重 PH(即HVPG ≥16 mmHg)。然后,MLM 在各个外部数据集中进行评估,并在合并的队列中进行优化。
结果
在 1,232 名 cACLD 参与者中,维也纳队列(n = 163,67.4%/35.0%)和验证队列(n = 1,069,70.3%/34.7%)中 CSPH/严重 PH 的患病率相似。 MLM 基于 3 个(3P:血小板计数、胆红素、国际标准化比率)或 5 个(5P:+胆碱酯酶、+γ-谷氨酰转移酶、+取代国际标准化比率的活化部分凝血活酶时间)实验室参数。传销在维也纳队列中表现强劲。 5P-MLM 对于 CSPH (0.813) 和严重 PH (0.887) 具有最佳 AUC,并且与肝脏硬度测量 (AUC: 0.808) 相比毫不逊色。它们在外部验证数据集中的表现是异构的(AUC:0.589-0.887)。合并队列的训练优化了 CSPH(3P 和 5P 的 AUC:分别为 0.775 和 0.789)和严重 PH(分别为 0.737 和 0.828)的模型性能。
结论
内部训练的 MLM 可靠地预测了维也纳 cACLD 队列中的 PH 严重程度,但在外部验证中表现出异质性结果。所提出的 3P/5P 在线工具可以可靠地识别患有 CSPH 或严重 PH 的个体,因此他们有肝代偿失调的风险。
影响和影响
我们使用基于广泛可用的实验室参数的机器学习模型来开发一种无创模型来预测代偿性肝硬化患者门静脉高压的严重程度,这些患者目前需要对肝静脉压力梯度进行侵入性测量。我们在一个大型多中心队列中验证了我们的研究结果,该队列由患有任何原因的晚期慢性肝病 (cACLD) 的个体组成。最后,我们提供了一个现成的在线计算器,基于 3 个(血小板计数、胆红素、国际标准化比率)或 5 个(血小板计数、胆红素、活化部分凝血活酶时间、γ-谷氨酰转移酶、胆碱酯酶)广泛可用的实验室参数,临床医生可以用来预测 cACLD 患者患有临床显着或严重门静脉高压的可能性。











































 京公网安备 11010802027423号
京公网安备 11010802027423号