Biomedicine & Pharmacotherapy ( IF 6.9 ) Pub Date : 2022-09-20 , DOI: 10.1016/j.biopha.2022.113688 Song-Hee Kim 1 , Seung-Il Baek 1 , Jihye Jung 1 , Eung-Seok Lee 2 , Younghwa Na 3 , Bang Yeon Hwang 1 , Yoon-Seok Roh 1 , Jin Tae Hong 1 , Sang-Bae Han 1 , Youngsoo Kim 1
|
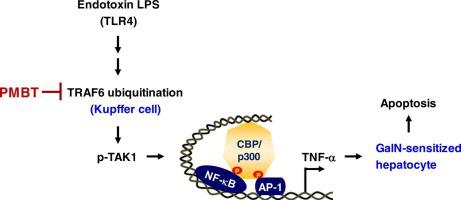
The liver is exposed to gut-derived bacterial endotoxin via portal circulation, and recognizes it through toll-like receptor 4 (TLR4). Endotoxin lipopolysaccharide (LPS) stimulates the self-ubiquitination of ubiquitin ligase TRAF6, which is linked to scaffold with protein kinase TAK1 for auto-phosphorylation and subsequent activation. TAK1 activity is a signal transducer in the activating pathways of transcription factors NF-κB and AP-1 for production of various cytokines. Here, we hypothesized that TRAF6-TAK1 axis would be implicated in endotoxin-induced liver disease. Following exposure to endotoxin LPS, TLR4-mediated phosphorylation of TAK1 and transcription of cell-death cytokine TNF-α were triggered in Kupffer cells but not in hepatocytes as well as TNF receptor-mediated and caspase-3-executed apoptosis was occurred in D-galactosamine (GalN)-sensitized hepatocytes under co-culture with Kupffer cells. Treatment with pyridinylmethylene benzothiophene (PMBT) improved endotoxin LPS-induced hepatocyte apoptosis in GalN-sensitized C57BL/6 mice via suppressing NF-κB- and AP-1-regulated expression of TNF-α in Kupffer cells, and rescued the mice from hepatic damage-associated bleeding and death. As a mechanism, PMBT directly inhibited Lys 63-linked ubiquitination of TRAF6, and mitigated scaffold assembly between TRAF6 and the TAK1-activator adaptors TAB1 and TAB2 complex in Kupffer cells. Thereby, PMBT interrupted TRAF6 ubiquitination-induced activation of TAK1 activity in the TLR4-mediated signal cascade leading to TNF-α production. However, PMBT did not directly affect the apoptotic activity of TNF-α on GalN-sensitized hepatocytes. Finally, we propose chemical inhibition of TRAF6-TAK1 axis in Kupffer cells as a strategy for treating liver disease due to gut-derived endotoxin or Gram-negative bacterial infection.
中文翻译:

化学抑制 TRAF6-TAK1 轴作为内毒素诱导肝病的治疗策略
肝脏通过门静脉循环暴露于肠道衍生的细菌内毒素,并通过 toll 样受体 4 (TLR4) 识别它。内毒素脂多糖 (LPS) 刺激泛素连接酶 TRAF6 的自泛素化,TRAF6 与蛋白激酶 TAK1 连接到支架上,用于自磷酸化和随后的激活。TAK1 活性是转录因子 NF-κB 和 AP-1 激活途径中的信号转导,用于产生各种细胞因子。在这里,我们假设 TRAF6-TAK1 轴与内毒素诱导的肝病有关。在暴露于内毒素 LPS 后,TLR4 介导的 TAK1 磷酸化和细胞死亡细胞因子 TNF-α 的转录在 Kupffer 细胞中被触发,但在肝细胞中没有被触发,以及 TNF 受体介导和 caspase-3 执行的细胞凋亡发生在D-半乳糖胺 (GalN) 致敏的肝细胞与枯否细胞共培养。吡啶基亚甲基苯并噻吩 (PMBT) 治疗通过抑制 Kupffer 细胞中 NF-κB 和 AP-1 调节的 TNF-α 表达,改善了内毒素 LPS 诱导的 GalN 致敏 C57BL/6 小鼠肝细胞凋亡,并挽救了小鼠的肝损伤-相关的出血和死亡。作为一种机制,PMBT 直接抑制了与赖氨酸 63 连接的 TRAF6 泛素化,并减轻了 Kupffer 细胞中 TRAF6 与 TAK1 激活剂接头 TAB1 和 TAB2 复合物之间的支架组装。因此,PMBT 在 TLR4 介导的信号级联中中断了 TRAF6 泛素化诱导的 TAK1 活性激活,从而导致 TNF-α 的产生。然而,PMBT 不直接影响 TNF-α 对 GalN 致敏肝细胞的凋亡活性。最后,











































 京公网安备 11010802027423号
京公网安备 11010802027423号