当前位置:
X-MOL 学术
›
Cancer Sci.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Combined chemoradiotherapy and programmed cell death-ligand 1 blockade leads to changes in the circulating T-cell receptor repertoire of patients with non-small-cell lung cancer
Cancer Science ( IF 4.5 ) Pub Date : 2022-09-07 , DOI: 10.1111/cas.15566 Masanori Someya 1 , Serina Tokita 2 , Takayuki Kanaseki 2 , Mio Kitagawa 1 , Tomokazu Hasegawa 1 , Takaaki Tsuchiya 1 , Yuki Fukushima 1 , Toshio Gocho 1 , Yoh Kozuka 1 , Shoh Mafune 1 , Yutaro Ikeuchi 1 , Mamoru Takahashi 3 , Keigo Moniwa 2, 3 , Kazuhiko Matsuo 4 , Tadashi Hasegawa 5 , Toshihiko Torigoe 2 , Koh-Ichi Sakata 1
Cancer Science ( IF 4.5 ) Pub Date : 2022-09-07 , DOI: 10.1111/cas.15566 Masanori Someya 1 , Serina Tokita 2 , Takayuki Kanaseki 2 , Mio Kitagawa 1 , Tomokazu Hasegawa 1 , Takaaki Tsuchiya 1 , Yuki Fukushima 1 , Toshio Gocho 1 , Yoh Kozuka 1 , Shoh Mafune 1 , Yutaro Ikeuchi 1 , Mamoru Takahashi 3 , Keigo Moniwa 2, 3 , Kazuhiko Matsuo 4 , Tadashi Hasegawa 5 , Toshihiko Torigoe 2 , Koh-Ichi Sakata 1
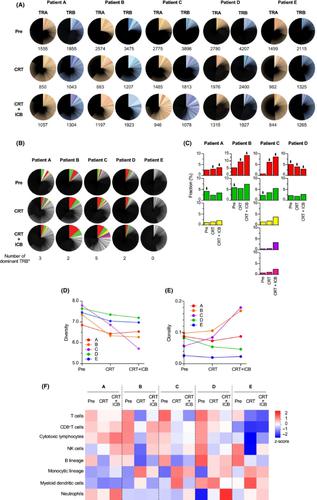
Affiliation
|
Combined chemoradiotherapy (CRT) and programmed cell death-ligand 1 (PD-L1) blockade is a new care standard for unresectable stage III non-small-cell lung cancer (NSCLC). Although this consolidation therapy has improved the overall survival of patients with NSCLC, the synergistic action mechanisms of CRT and immunotherapy on T cells remain unclear. In addition, there is a paucity of reliable biomarkers to predict clinical responses to therapy. In this study, we analyzed T-cell receptor (TCR) sequences in the peripheral blood of five patients with NSCLC. T-cell receptor analysis was undertaken before treatment, after CRT, and after PD-L1 blockade. Notably, we observed the expansion and alteration of the dominant T-cell clonotypes in all cases with a complete response. In contrast, neither expansion nor alteration of the TCR repertoire was observed in cases with progressive disease. T cell expansion was initiated after CRT and was further enhanced after PD-L1 blockade. Our findings suggest the systemic effect of CRT on circulating T cells in addition to the curative effect on limited tumor sites. Dynamic changes in circulating T-cell clonotypes could have a prognostic significance for combined CRT and PD-L1 blockade.
中文翻译:

联合放化疗和程序性细胞死亡-配体 1 阻断导致非小细胞肺癌患者循环 T 细胞受体库发生变化
联合放化疗 (CRT) 和程序性细胞死亡配体 1 (PD-L1) 阻断是不可切除的 III 期非小细胞肺癌 (NSCLC) 的新护理标准。虽然这种巩固治疗改善了NSCLC患者的总生存期,但CRT和免疫治疗对T细胞的协同作用机制仍不清楚。此外,缺乏可靠的生物标志物来预测临床对治疗的反应。在这项研究中,我们分析了五名非小细胞肺癌患者外周血中的 T 细胞受体 (TCR) 序列。在治疗前、CRT 后和 PD-L1 阻断后进行 T 细胞受体分析。值得注意的是,我们观察到在所有具有完全反应的病例中显性 T 细胞克隆型的扩增和改变。相比之下,在疾病进展的病例中,既没有观察到 TCR 库的扩展也没有改变。CRT 后启动 T 细胞扩增,并在 PD-L1 阻断后进一步增强。我们的研究结果表明,除了对有限的肿瘤部位有疗效外,CRT 对循环 T 细胞的全身作用。循环 T 细胞克隆型的动态变化可能对联合 CRT 和 PD-L1 阻断具有预后意义。
更新日期:2022-09-07
中文翻译:

联合放化疗和程序性细胞死亡-配体 1 阻断导致非小细胞肺癌患者循环 T 细胞受体库发生变化
联合放化疗 (CRT) 和程序性细胞死亡配体 1 (PD-L1) 阻断是不可切除的 III 期非小细胞肺癌 (NSCLC) 的新护理标准。虽然这种巩固治疗改善了NSCLC患者的总生存期,但CRT和免疫治疗对T细胞的协同作用机制仍不清楚。此外,缺乏可靠的生物标志物来预测临床对治疗的反应。在这项研究中,我们分析了五名非小细胞肺癌患者外周血中的 T 细胞受体 (TCR) 序列。在治疗前、CRT 后和 PD-L1 阻断后进行 T 细胞受体分析。值得注意的是,我们观察到在所有具有完全反应的病例中显性 T 细胞克隆型的扩增和改变。相比之下,在疾病进展的病例中,既没有观察到 TCR 库的扩展也没有改变。CRT 后启动 T 细胞扩增,并在 PD-L1 阻断后进一步增强。我们的研究结果表明,除了对有限的肿瘤部位有疗效外,CRT 对循环 T 细胞的全身作用。循环 T 细胞克隆型的动态变化可能对联合 CRT 和 PD-L1 阻断具有预后意义。









































 京公网安备 11010802027423号
京公网安备 11010802027423号