Clinical Gastroenterology and Hepatology ( IF 11.6 ) Pub Date : 2022-08-31 , DOI: 10.1016/j.cgh.2022.08.024 Remi Mahmoud 1 , Edo H J Savelkoul 2 , Wout Mares 3 , Rogier Goetgebuer 4 , Ben J M Witteman 3 , Daan B de Koning 5 , Sebastiaan A C van Tuyl 6 , Itta Minderhoud 7 , Maurice W M D Lutgens 8 , Dilek Akol-Simsek 9 , Fiona D M van Schaik 1 , Herma H Fidder 1 , Jeroen M Jansen 10 , Petra G A van Boeckel 11 , Nofel Mahmmod 11 , Carmen S Horjus-Talabur Horje 12 , Tessa E H Römkens 13 , Jean-Frédéric Colombel 14 , Frank Hoentjen 15 , Bindia Jharap 16 , Bas Oldenburg 1 ,
|
Background & Aims
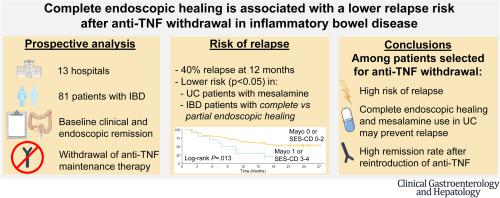
Discontinuation of anti–tumor necrosis factor-α treatment (anti-TNF) (infliximab and adalimumab) in patients with inflammatory bowel disease (IBD) is associated with a high relapse risk that may be influenced by endoscopic activity at the time of stopping. We assessed the relapse rate after anti-TNF withdrawal in patients with endoscopic healing and studied predictors of relapse including the depth of endoscopic healing.
Methods
This was a multicenter, prospective study in adult patients with Crohn’s disease (CD), ulcerative colitis (UC), or IBD-unclassified (IBDU), with ≥6 months of corticosteroid-free clinical remission (confirmed at baseline) and endoscopic healing (Mayo <2/SES-CD <5 without large ulcers), who discontinued anti-TNF between 2018 and 2020 in the Netherlands. We performed Kaplan-Meier and Cox regression analyses to assess the relapse rate and evaluate potential predictors: partial (Mayo 1/SES-CD 3–4) versus complete (Mayo 0/SES-CD 0–2) endoscopic healing, anti-TNF trough levels, and immunomodulator and/or mesalamine use.
Results
Among 81 patients (CD: n = 41, 51%) with a median follow-up of 2.0 years (interquartile range, 1.6–2.1), 40 patients (49%) relapsed. Relapse rates in CD and UC/IBDU patients were comparable. At 12 months, 70% versus 35% of patients with partial versus complete endoscopic healing relapsed, respectively (adjusted hazard rate [aHR], 3.28; 95% confidence interval [CI], 1.43–7.50). Mesalamine use was associated with fewer relapses in UC/IBDU patients (aHR, 0.08; 95% CI, 0.01–0.67). Thirty patients restarted anti-TNF, and clinical remission was regained in 73% at 3 months.
Conclusions
The relapse risk was high after anti-TNF withdrawal in IBD patients with endoscopic healing, but remission was regained in most cases after anti-TNF reintroduction. Complete endoscopic healing and mesalamine treatment in UC/IBDU patients decreased the risk of relapse.
中文翻译:

炎症性肠病抗肿瘤坏死因子撤药后,内镜下完全愈合与较低的复发风险相关
背景与目标
炎症性肠病 (IBD) 患者停止抗肿瘤坏死因子-α 治疗(抗 TNF)(英夫利昔单抗和阿达木单抗)与高复发风险相关,这可能受停止时内镜活动的影响。我们评估了内镜愈合患者停用抗 TNF 后的复发率,并研究了包括内镜愈合深度在内的复发预测因子。
方法
这是一项针对患有克罗恩病 (CD)、溃疡性结肠炎 (UC) 或未分类 IBD (IBDU) 的成年患者的多中心、前瞻性研究,具有≥6 个月的无皮质类固醇临床缓解(在基线时确认)和内窥镜愈合( Mayo <2/SES-CD <5,无大溃疡),他们在 2018 年至 2020 年间在荷兰停止了抗 TNF 治疗。我们进行了 Kaplan-Meier 和 Cox 回归分析以评估复发率并评估潜在预测因子:部分(Mayo 1/SES-CD 3-4)与完全(Mayo 0/SES-CD 0-2)内窥镜愈合、抗 TNF谷水平、免疫调节剂和/或美沙拉嗪的使用。
结果
在 81 名患者 (CD: n = 41, 51%) 中位随访 2.0 年(四分位间距,1.6–2.1)中,40 名患者 (49%) 复发。CD 和 UC/IBDU 患者的复发率相当。在 12 个月时,内镜下部分愈合和完全愈合的患者分别有 70% 和 35% 复发(调整后的风险率 [aHR],3.28;95% 置信区间 [CI],1.43–7.50)。使用美沙拉嗪与 UC/IBDU 患者的较少复发相关(aHR,0.08;95% CI,0.01–0.67)。30 名患者重新开始抗肿瘤坏死因子治疗,3 个月时有 73% 的患者恢复了临床缓解。
结论
在内镜下治愈的 IBD 患者停用抗 TNF 后复发风险很高,但大多数病例在重新引入抗 TNF 后恢复缓解。UC/IBDU 患者的完全内镜愈合和美沙拉嗪治疗降低了复发风险。











































 京公网安备 11010802027423号
京公网安备 11010802027423号