Drugs in R&D ( IF 2.2 ) Pub Date : 2022-08-20 , DOI: 10.1007/s40268-022-00399-y Maki Umemiya 1 , Yoshihide Inayama 1, 2 , Eiji Nakatani 3 , Kenta Ito 4 , Mitsuru Tsuji 1 , Teruki Yoshida 1 , Sae Yu 1 , Rei Gou 1 , Naoki Horikawa 1 , Hirohiko Tani 1 , Kenzo Kosaka 1
|
Background and Objectives
Irinotecan sometimes causes lethal septic shock but the risk factors remain unclear. This retrospective case-control study explored the potential risk factors for septic shock following irinotecan treatment.
Methods
All women who received irinotecan-containing chemotherapy for gynecologic malignancies at Shizuoka General Hospital from October 2014 to September 2020 were investigated. The clinical backgrounds and blood test results of those who developed septic shock after irinotecan-containing chemotherapy were compared with those who did not. Odds ratios (ORs) for developing septic shock after receiving irinotecan were calculated with 95% confidence intervals (CIs), using univariable logistic regression analysis.
Results
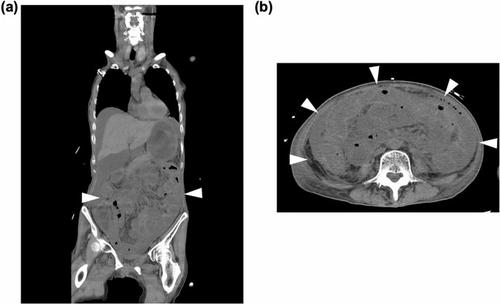
During the study period, 147 women received irinotecan-containing chemotherapy. Three women developed septic shock due to neutropenic enterocolitis after irinotecan treatment, and 144 did not. The three patients with septic shock had recurrent cervical cancer, heterozygous variants in the uridine diphosphate glucuronosyltransferase 1A1 (UGT1A1) gene (two patients had *1/*6, one had *1/*28 variants), a history of concurrent chemoradiation therapy, 50–60 Gy of pelvic irradiation, and platinum-combined chemotherapy. A history of pelvic irradiation was identified as a possible risk factor for developing septic shock after irinotecan-containing chemotherapy (OR 63.0, 95% CI 5.71–8635; p < 0.001). The OR of UGT1A1 polymorphism for septic shock was 9.09 (95% CI 0.86–1233; p = 0.070) in the complete case analysis.
Conclusion
Medical personnel involved in cancer therapy should consider the possible risk of septic shock developing due to neutropenic enterocolitis when administering irinotecan-containing chemotherapy in patients with a history of pelvic irradiation.
中文翻译:

伊立替康化疗后感染性休克的危险因素:一项探索性病例对照研究
背景和目标
伊立替康有时会导致致命的感染性休克,但风险因素仍不清楚。这项回顾性病例对照研究探讨了伊立替康治疗后感染性休克的潜在危险因素。
方法
调查了 2014 年 10 月至 2020 年 9 月期间在静冈综合医院接受含伊立替康化疗治疗妇科恶性肿瘤的所有女性。将含伊立替康化疗后发生感染性休克的患者的临床背景和血液检查结果与未发生的患者进行比较。使用单变量逻辑回归分析计算接受伊立替康后发生感染性休克的优势比 (OR) 和 95% 置信区间 (CI)。
结果
在研究期间,147 名女性接受了含伊立替康的化疗。3 名女性在伊立替康治疗后因中性粒细胞减少性小肠结肠炎出现感染性休克,而 144 名则没有。三例感染性休克患者有复发性宫颈癌,尿苷二磷酸葡萄糖醛酸转移酶 1A1 ( UGT1A1 ) 基因杂合变异(两名患者有*1/ *6,一名有*1/*28变异),有同步放化疗史, 50-60 Gy 的盆腔照射和铂类联合化疗。盆腔放疗史被确定为含伊立替康化疗后发生感染性休克的可能危险因素(OR 63.0,95% CI 5.71–8635;p < 0.001)。UGT1A1的或 在完整病例分析中,感染性休克的多态性为 9.09(95% CI 0.86–1233;p = 0.070)。
结论
参与癌症治疗的医务人员在对有盆腔放疗史的患者进行含伊立替康的化疗时,应考虑到中性粒细胞减少性小肠结肠炎可能导致感染性休克的风险。










































 京公网安备 11010802027423号
京公网安备 11010802027423号