Gastroenterology ( IF 25.7 ) Pub Date : 2022-08-13 , DOI: 10.1053/j.gastro.2022.08.020 Keming Yang 1 , Yin Cao 2 , Carino Gurjao 3 , Yang Liu 4 , Chuan-Guo Guo 5 , Chun-Han Lo 6 , Xiaoyu Zong 7 , David Drew 6 , Connor Geraghty 6 , Elizabeth Prezioso 6 , Matt Moore 8 , Craig Williams 8 , Tom Riley 8 , Melissa Saul 9 , Shuji Ogino 10 , Marios Giannakis 11 , Adam Bass 12 , Robert E Schoen 13 , Andrew T Chan 14
|
Background & Aims
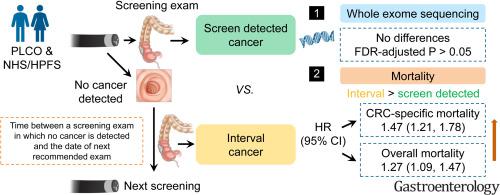
Interval colorectal cancers (CRCs), cancers diagnosed after a screening/surveillance examination in which no cancer is detected, and before the date of next recommended examination, reflect an unprecedented challenge in CRC detection and prevention. To better understand this poorly characterized CRC variant, we examined the clinical and mutational characteristics of interval CRCs in comparison with screen detected CRCs.
Methods
We included 1175 CRCs documented in the Prostate, Lung, Colorectal, and Ovarian (PLCO) cancer screening trial and 3661 CRCs in the Nurses’ Health Study (NHS) and Health Professionals Follow-up Study (HPFS). Multivariable Cox models were performed to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) of death risk. Whole exome sequencing was conducted in 147 PLCO cases and 796 NHS/HPFS cases.
Results
A total of 619 deaths (312 CRC-specific) and 2404 deaths (1904 CRC-specific) were confirmed during follow-up of PLCO and NHS/HPFS, respectively. Compared with screen detected CRCs, interval CRCs had a multivariate-adjusted HR (95% CI) of 1.47 (1.21–1.78) for CRC-specific mortality and 1.27 (1.09–1.47) for overall mortality (meta-analysis combining all 3 cohorts). However, we did not observe significant differences in mutational features between interval and screen detected CRCs (false discovery rate adjusted P > .05).
Conclusion
Interval CRCs had a significantly increased risk of death compared with screen detected CRCs that were not explained by established clinical prognostic factors, including stage at diagnosis. The survival disadvantage of interval CRCs did not appear to be explained by differences in the genomic landscape of tumors characterized by whole exome sequencing.
中文翻译:

3 个前瞻性队列中间期结直肠癌的临床和基因组特征
背景与目标
间期结直肠癌 (CRC) 是在筛查/监测检查后未检测到癌症且在下次推荐检查日期之前诊断出的癌症,反映了 CRC 检测和预防方面前所未有的挑战。为了更好地了解这种特征不明的 CRC 变异,我们检查了间期 CRC 的临床和突变特征,并与筛查检测到的 CRC 进行了比较。
方法
我们纳入了前列腺癌、肺癌、结直肠癌和卵巢癌 (PLCO) 癌症筛查试验中记录的 1175 例 CRC,以及护士健康研究 (NHS) 和卫生专业人员随访研究 (HPFS) 中记录的 3661 例 CRC。采用多变量 Cox 模型来估计死亡风险的危险比 (HR) 和 95% 置信区间 (CI)。对 147 例 PLCO 病例和 796 例 NHS/HPFS 病例进行了全外显子组测序。
结果
在 PLCO 和 NHS/HPFS 的随访期间,分别确认了 619 例死亡(312 例 CRC 特异性)和 2404 例死亡(1904 例 CRC 特异性)。与筛查检测到的 CRC 相比,间期 CRC 的 CRC 特异性死亡率的多变量调整 HR (95% CI) 为 1.47 (1.21–1.78),总死亡率为 1.27 (1.09–1.47)(结合所有 3 个队列的荟萃分析) 。然而,我们没有观察到间隔检测和筛选检测的 CRC 之间突变特征的显着差异(错误发现率调整后P > .05)。
结论
与筛查检测到的 CRC 相比,间期 CRC 的死亡风险显着增加,且无法用既定的临床预后因素(包括诊断时的分期)来解释。间期CRC的生存劣势似乎不能用全外显子组测序表征的肿瘤基因组景观的差异来解释。











































 京公网安备 11010802027423号
京公网安备 11010802027423号