American Journal of Kidney Diseases ( IF 9.4 ) Pub Date : 2022-08-07 , DOI: 10.1053/j.ajkd.2022.06.009 Navneet Singh 1 , Punithan Thiagalingam 1 , Junayd Hussain 1 , Vishva Shah 1 , Nathaniel Edwards 1 , Eric Lui 1 , Gihad Nesrallah 2 , Charmaine E Lok 3 , Abdul Aziz Walele 4 , Marta Novak 5 , Carl E James 6 , Istvan Mucsi 1
|
Rationale & Objective
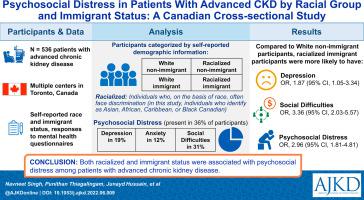
Patients with advanced chronic kidney disease (CKD) have been reported to experience profound psychosocial distress. Other work has established that patients with CKD from marginalized populations (including individuals who on the basis of race often face racism and related discrimination, termed “racialization”) experience health care inequities. Given limited information on the intersection of these 2 phenomena, we assessed the association of psychosocial distress with racialized status and immigrant status in Canadians with advanced CKD.
Study Design
Secondary analysis of cross-sectional data.
Setting & Participants
536 patients with advanced CKD (estimated glomerular filtration rate < 30 mL/min/1.73 m2, with or without kidney replacement therapy) from multiple clinical centers in Toronto.
Exposure
Racialized status (individuals who identify as Asian or as African, Caribbean, or Black Canadian), immigrant status, and combined immigrant-racialized status.
Outcome
Psychosocial distress, defined as the presence of depression, anxiety, or social difficulties (ie, a score of ≥10 points on the Patient Health Questionnaire 9, Generalized Anxiety Disorder 7, or Social Distress 16 scales, respectively).
Analytical Approach
The independent associations of racialized status and immigrant status with psychosocial distress, depression, anxiety, and social difficulties were examined using univariable- and multivariable-adjusted logistic regression.
Results
Mean age of the 536 participants was 57 ± 16 (SD) years, 62% were male, and 45% were immigrants. Of the sample, 58% were White, 22% were African, Caribbean, or Black Canadian, and 20% were Asian. Psychosocial distress was present in 36% of participants (depression in 19%, anxiety in 12%, and social difficulties in 31%). To assess the combined impact of racialized and immigrant status, we created a variable with mutually exclusive categories: White nonimmigrant, racialized nonimmigrant, White immigrant, and racialized immigrant participants. In our final multivariable-adjusted model, compared with White nonimmigrant participants, racialized immigrant participants were more likely to have psychosocial distress (OR, 2.96 [95% CI, 1.81-4.81]), depression (OR, 1.87 [95% CI, 1.05-3.34]), and social difficulties (OR, 3.36 [95% CI, 2.03-5.57]). Overall similar associations were seen for racialized nonimmigrants and for White immigrants.
Limitations
Convenience sample; small subgroups; combined exposure variable grouping Asian and African, Caribbean, and Black participants together; lack of data about mechanisms.
Conclusions
Both racialized and immigrant status based on self-report of demographic characteristics were associated with psychosocial distress among patients with advanced CKD. These patients may benefit from culturally competent psychosocial support.
Plain-Language Summary
Psychosocial distress is frequent in patients with advanced chronic kidney disease and impacts quality of life and clinical outcomes. Psychosocial distress may be especially scarring in people who are racialized (marginalized on account of their membership in a particular racial group) and/or who are immigrants. We assessed the association of psychosocial distress with racialized and immigrant status in Canadians with advanced chronic kidney disease. Among 536 participants from multiple medical centers in Toronto, we found that racialized and immigrant participants were more likely to have psychosocial distress, depression, and social difficulties compared with White nonimmigrant participants. This is likely related to the multiple intersectional challenges, including experience with racism and discrimination that racialized immigrant patients may face. Further studies are needed to elucidate the specific factors that contribute to more distress. The potential impact of culturally competent and safe support for these patients will also need to be studied.
中文翻译:

不同种族和移民身份的晚期 CKD 患者的社会心理压力:一项加拿大横断面研究
理由和目标
据报道,患有晚期慢性肾脏病 (CKD) 的患者会经历严重的社会心理困扰。其他工作已经确定来自边缘化人群(包括基于种族经常面临种族主义和相关歧视,称为“种族化”)的 CKD 患者经历了医疗保健不平等。鉴于关于这两种现象交集的信息有限,我们评估了患有晚期 CKD 的加拿大人的社会心理困扰与种族化身份和移民身份之间的关联。
学习规划
横截面数据的二次分析。
设置和参与者
来自多伦多多个临床中心的536 名晚期 CKD 患者(估计肾小球滤过率 < 30 mL/min/1.73 m 2 ,接受或不接受肾脏替代治疗)。
接触
种族化身份(被认定为亚洲人或非洲人、加勒比海地区或加拿大黑人的个人)、移民身份以及移民-种族化身份的结合。
结果
社会心理困扰,定义为存在抑郁、焦虑或社交困难(即 患者健康问卷 9、广泛性焦虑症 7 或社交困扰 16 量表的得分分别≥10 分)。
分析方法
使用单变量和多变量调整后的逻辑回归检查种族化地位和移民地位与社会心理困扰、抑郁、焦虑和社交困难的独立关联。
结果
536 名参与者的平均年龄为 57 ± 16 (SD) 岁,62% 为男性,45% 为移民。在样本中,58% 是白人,22% 是非洲人、加勒比人或加拿大黑人,20% 是亚裔。36% 的参与者存在社会心理困扰(抑郁症占 19%,焦虑症占 12%,社交困难占 31%)。为了评估种族化和移民身份的综合影响,我们创建了一个具有相互排斥类别的变量:白人非移民、种族化非移民、白人移民和种族化移民参与者。在我们最终的多变量调整模型中,与白人非移民参与者相比,种族化的移民参与者更有可能出现社会心理困扰(OR,2.96 [95% CI,1.81-4.81])、抑郁症(OR,1.87 [95% CI,1.05] -3.34])和社交困难(OR,3.36 [95% CI,2.03-5.57])。
限制
方便样品;小的子群;将亚洲和非洲、加勒比地区和黑人参与者组合在一起的暴露变量组合;缺乏有关机制的数据。
结论
基于自我报告的人口统计特征的种族化和移民身份都与晚期 CKD 患者的社会心理困扰有关。这些患者可能受益于具有文化能力的社会心理支持。
通俗易懂的摘要
晚期慢性肾病患者经常出现社会心理困扰,并影响生活质量和临床结果。对于种族化(由于属于特定种族群体而被边缘化)和/或移民的人来说,社会心理困扰可能尤其严重。我们评估了患有晚期慢性肾病的加拿大人的社会心理困扰与种族化和移民身份之间的关系。在来自多伦多多个医疗中心的 536 名参与者中,我们发现与白人非移民参与者相比,种族化和移民参与者更容易出现社会心理困扰、抑郁和社交困难。这可能与多重交叉挑战有关,包括种族化移民患者可能面临的种族主义和歧视的经历。需要进一步的研究来阐明导致更多痛苦的具体因素。还需要研究文化能力和安全支持对这些患者的潜在影响。











































 京公网安备 11010802027423号
京公网安备 11010802027423号