Clinical Gastroenterology and Hepatology ( IF 12.6 ) Pub Date : 2022-08-05 , DOI: 10.1016/j.cgh.2022.07.028 Aaron Yeoh 1 , Ajitha Mannalithara 1 , Uri Ladabaum 1
|
Background & Aims
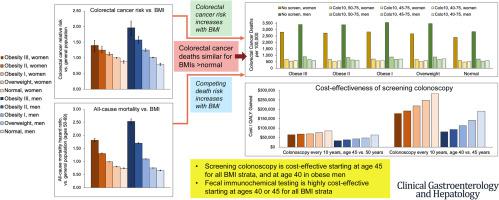
Overweight and obese persons have not only elevated rates of colorectal cancer (CRC), but also higher competing mortality and healthcare spending. We examined the cost-effectiveness of intensified CRC screening in overweight and obese persons.
Methods
We adapted our validated decision analytic model of CRC screening to compare screening starting at 45 or 40 years of age instead of at 50 years of age, or shortening screening intervals, in women and men with body mass index (BMI) ranging from normal to grade III obesity. Strategies included colonoscopy every 10 years (Colo10) or every 5 years (Colo5), or annual fecal immunochemical test.
Results
Without screening, sex-specific total CRC deaths were similar for persons with overweight or obesity I–III, reflecting the counterbalancing of higher CRC risk by lower life expectancy as BMI rises. For all BMI and sex groups, Colo10 starting at 45 years of age or FIT starting at 40 years of age were cost-effective at a threshold of $100,000 per quality-adjusted life year gained. Colo10 starting at 40 years of age was cost-effective only for men with obesity II–III, at $93,300 and $80,400 per quality-adjusted life year gained, respectively. Shifting Colo10 to earlier starting ages was always preferred over Colo5 starting at later ages. Results were robust in sensitivity analysis, including varying all-cause mortality, complication, and BMI-specific CRC risks.
Conclusions
CRC screening starting at 45 years of age with colonoscopy, or at 40 years of age with FIT, appears cost-effective for women and men across the range of BMI. In men with obesity II–III, who have the highest CRC but also all-cause mortality risks, colonoscopy starting at 40 years of age appears cost-effective. It remains to be decided whether BMI should be used as a single predictor or incorporated into a multivariable tool to tailor CRC screening.
中文翻译:

对超重和肥胖患者进行早期或更深入的结直肠癌筛查的成本效益
背景与目标
超重和肥胖的人不仅会增加结直肠癌 (CRC) 的发病率,还会增加死亡率和医疗保健支出。我们检查了在超重和肥胖人群中强化 CRC 筛查的成本效益。
方法
我们调整了经过验证的 CRC 筛查决策分析模型,以比较从 45 岁或 40 岁开始而不是从 50 岁开始筛查,或缩短筛查间隔,对体重指数 (BMI) 从正常到等级不等的女性和男性进行比较三、肥胖。策略包括每 10 年 (Colo10) 或每 5 年 (Colo5) 进行一次结肠镜检查,或每年进行一次粪便免疫化学测试。
结果
在没有筛查的情况下,超重或肥胖 I-III 人群的性别特异性 CRC 总死亡数相似,反映出随着 BMI 升高,CRC 风险增加与预期寿命降低相抵消。对于所有 BMI 和性别组,从 45 岁开始的 Colo10 或从 40 岁开始的 FIT 在每获得质量调整生命年 100,000 美元的阈值下具有成本效益。从 40 岁开始使用 Colo10 仅对 II-III 型肥胖男性具有成本效益,每增加一个质量调整生命年分别为 93,300 美元和 80,400 美元。将 Colo10 转移到更早的开始年龄总是比从更晚的年龄开始的 Colo5 更受欢迎。结果在敏感性分析中是稳健的,包括不同的全因死亡率、并发症和 BMI 特定的 CRC 风险。
结论
CRC 筛查从 45 岁开始使用结肠镜检查,或从 40 岁开始使用 FIT,对于不同 BMI 范围内的女性和男性来说似乎具有成本效益。对于具有最高 CRC 但全因死亡风险的 II-III 型肥胖男性,从 40 岁开始进行结肠镜检查似乎具有成本效益。BMI 是否应该用作单一预测因子或纳入多变量工具以定制 CRC 筛查仍有待决定。



























 京公网安备 11010802027423号
京公网安备 11010802027423号