Clinical Gastroenterology and Hepatology ( IF 12.6 ) Pub Date : 2022-07-19 , DOI: 10.1016/j.cgh.2022.06.029 Ansel Tang 1 , Cheng Han Ng 1 , Poh Hui Phang 1 , Kai En Chan 1 , Yip Han Chin 1 , Clarissa Elysia Fu 1 , Rebecca Wenling Zeng 1 , Jieling Xiao 1 , Darren Jun Hao Tan 1 , Jingxuan Quek 1 , Wen Hui Lim 1 , Lung Yi Mak 2 , Jiong-Wei Wang 3 , Nicholas W S Chew 4 , Nicholas Syn 1 , Daniel Q Huang 5 , Mohammad Shadab Siddiqui 6 , Arun Sanyal 6 , Mark Muthiah 5 , Mazen Noureddin 7
|
Background
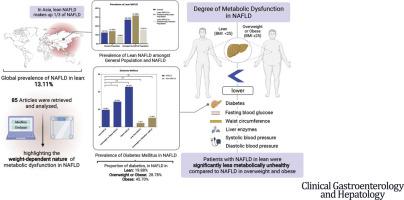
Nonalcoholic fatty liver disease (NAFLD) is traditionally associated with obesity. However, there is a subtype of NAFLD, namely NAFLD in lean, that occurs without obesity. However, a recent call to redefine NAFLD to metabolic associated fatty liver disease (MAFLD) focuses on obesity and metabolic dysfunction. Criticism has arisen from the perceived over emphasis on systemic comorbidities, which may disadvantage the lean. The current analysis seeks to quantify the degree of metabolic dysfunction in NAFLD in lean and compare with NAFLD in overweight and obese and non-NAFLD.
Methods
Medline and Embase databases were searched from inception to 3 March 2022. The inclusion criteria were articles with NAFLD in lean patients presenting with baseline metabolic parameters. Comparisons were conducted with subgroup analysis.
Results
Eighty-five articles were included in the meta-analysis. NAFLD in lean accounted for 13.11% (CI: 10.26%-16.62%) of the global population and 14.55% (CI: 11.32%–18.51%) in Asia. The degree of metabolic dysfunction was weight dependent with significantly less metabolic dysfunction in NAFLD in lean subjects as compared to NAFLD in overweight counterparts. For NAFLD in lean, only 19.56% (CI: 15.28–24.69) of the subjects were diabetic while 45.70% (CI: 35.01%-56.80%) of obese subjects with NAFLD had diabetes (p<0.01). Fasting blood glucose, systolic and diastolic blood pressure values were significantly lower in subjects with NAFLD in lean than in overweight and obese.
Conclusion
The current analysis highlights the weight-dependent nature of metabolic dysfunction in NAFLD. Lean subjects with NAFLD were significantly less metabolically unhealthy than were obese and overweight persons with NAFLD. An overreliance on metabolic dysfunction in defining fatty liver will be a flaw in potentially excluding previously characterized NAFLD.
中文翻译:

瘦型 NAFLD 与非瘦型 NAFLD 的代谢功能障碍负担比较 - 系统回顾和荟萃分析
背景
非酒精性脂肪肝(NAFLD)传统上与肥胖有关。然而,NAFLD 有一种亚型,即瘦型 NAFLD,这种亚型不会发生肥胖。然而,最近有人呼吁将 NAFLD 重新定义为代谢相关脂肪肝病 (MAFLD),重点关注肥胖和代谢功能障碍。批评源于人们认为过度强调系统性合并症,这可能对瘦身不利。目前的分析旨在量化瘦人 NAFLD 中代谢功能障碍的程度,并与超重、肥胖和非 NAFLD 中的 NAFLD 进行比较。
方法
Medline 和 Embase 数据库的搜索时间从开始到 2022 年 3 月 3 日。纳入标准是具有基线代谢参数的瘦患者的 NAFLD 文章。通过亚组分析进行比较。
结果
荟萃分析中纳入了 85 篇文章。瘦人 NAFLD 占全球人口的 13.11%(CI:10.26%-16.62%),在亚洲占 14.55%(CI:11.32%-18.51%)。代谢功能障碍的程度与体重相关,与超重受试者的 NAFLD 相比,瘦受试者的 NAFLD 代谢功能障碍明显减少。对于瘦 NAFLD 患者,只有 19.56%(CI:15.28-24.69)的受试者患有糖尿病,而 45.70%(CI:35.01%-56.80%)的肥胖 NAFLD 受试者患有糖尿病(p<0.01)。瘦 NAFLD 受试者的空腹血糖、收缩压和舒张压值显着低于超重和肥胖者。
结论
目前的分析强调了 NAFLD 代谢功能障碍的体重依赖性。患有 NAFLD 的瘦弱受试者的代谢不健康程度明显低于患有 NAFLD 的肥胖和超重受试者。过度依赖代谢功能障碍来定义脂肪肝可能会成为排除先前描述的 NAFLD 的缺陷。



























 京公网安备 11010802027423号
京公网安备 11010802027423号