The Journal of Thoracic and Cardiovascular Surgery ( IF 4.9 ) Pub Date : 2022-06-24 , DOI: 10.1016/j.jtcvs.2022.06.011 Junyi Yu 1 , Che Xu 2 , Zongmei Wen 3 , Guifang Wang 4 , Agustin Alejandro Gil Silva 5 , Mark J Brown 5 , Pablo G Sanchez 6 , Xingan Wang 7
|
Objectives
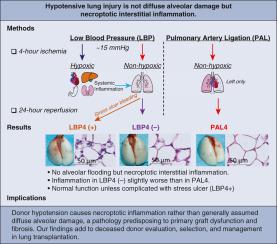
Hypotension episodes before or after donor brain death are assumed to trigger hypoxia-reoxygenation, causing diffuse alveolar-capillary damage via necrosis. However, alveolar-capillary membranes have direct access to oxygen in alveoli. We hypothesized hypotension-induced lung injury is not diffuse alveolar-capillary damage but interstitial inflammation resulting from nonhypoxic lung ischemia and systemic responses to hypoxic extrapulmonary ischemia.
Methods
The 4-hour hypotension model was established by subjecting C57BL/6J mice to 4-hour hypotension at 15 ± 5 mm Hg of mean artery pressure and resuscitated with whole shed blood and norepinephrine. Nonhypoxic lung ischemia model was established by 4-hour left pulmonary artery ligation. At 24 hours postprocedure, an arterial blood gas analysis and a gastroduodenal occult blood test were conducted. Lung samples were assessed for histology, cytokine transcripts, regulated cell death, and alveolar-capillary permeability.
Results
The 4-hour hypotension model had an intraoperative mortality rate of 17.7% (41/231) and a stress-ulcer bleeding rate of 15.3% (29/190). No signs of alveolar flooding were observed in both models. Four-hour hypotension without stress ulcer showed normal oxygenation and permeability but increased interstitial infiltration, transcription of Tnf and Il1b, phosphorylation of MLKL and RIPK3, and cleaved caspase 3 compared with 4-hour pulmonary artery ligation and naïve control. Animals that developed stress ulcer presented with worse pulmonary infiltration, intracellular edema, and oxygenation but just slightly increased permeability. Immunoblotting showed significant upregulations of protein expression and phosphorylation of MLKL and RIPK3, cleaved Caspase-3, but not its prototype in 4-hour hypotension with stress ulcer.
Conclusions
Hypotensive lung injury is essentially a nonhypoxic ischemia–reperfusion injury enhanced by systemic responses. It is predominated by necroptosis-induced inflammation rather than necrosis-induced diffuse alveolar-capillary damage.
中文翻译:

休克肺不是“湿的”,而是在低血压小鼠模型中表现为坏死性炎症
目标
假设供体脑死亡之前或之后的低血压发作会触发缺氧复氧,通过坏死引起弥漫性肺泡毛细血管损伤。然而,肺泡毛细血管膜可以直接接触肺泡中的氧气。我们假设低血压引起的肺损伤不是弥漫性肺泡毛细血管损伤,而是非缺氧性肺缺血和对缺氧性肺外缺血的全身反应引起的间质性炎症。
方法
通过使 C57BL/6J 小鼠在 15 ± 5 mm Hg 的平均动脉压下进行 4 小时低血压并用全流血和去甲肾上腺素复苏,建立 4 小时低血压模型。结扎左肺动脉4小时,建立非缺氧肺缺血模型。术后 24 小时,进行动脉血气分析和胃十二指肠潜血试验。评估肺样本的组织学、细胞因子转录物、受调节的细胞死亡和肺泡-毛细血管通透性。
结果
4 小时低血压模型的术中死亡率为 17.7% (41/231),应激性溃疡出血率为 15.3% (29/190)。两种模型均未观察到肺泡积水的迹象。与 4 小时肺动脉结扎和幼稚对照相比,无应激性溃疡的 4 小时低血压显示正常氧合作用和通透性,但间质浸润、Tnf 和 Il1b 转录、MLKL和RIPK3磷酸化以及裂解半胱天冬酶 3 增加。发生应激性溃疡的动物表现出更严重的肺浸润、细胞内水肿和氧合作用,但通透性略有增加。免疫印迹显示 MLKL 和 RIPK3 的蛋白质表达和磷酸化显着上调,裂解的 Caspase-3,但在伴有应激性溃疡的 4 小时低血压中不是其原型。
结论
低血压性肺损伤本质上是一种由全身反应增强的非缺氧性缺血再灌注损伤。它主要由坏死性凋亡引起的炎症而不是坏死引起的弥漫性肺泡 - 毛细血管损伤。









































 京公网安备 11010802027423号
京公网安备 11010802027423号