Journal of Hepatology ( IF 26.8 ) Pub Date : 2022-06-23 , DOI: 10.1016/j.jhep.2022.06.014 Bingyuan Huang 1 , Zhuwan Lyu 1 , Qiwei Qian 1 , Yong Chen 1 , Jun Zhang 1 , Bo Li 1 , Yikang Li 1 , Jubo Liang 1 , Qiaoyan Liu 1 , You Li 1 , Ruiling Chen 1 , Min Lian 1 , Xiao Xiao 1 , Qi Miao 1 , Qixia Wang 1 , Jingyuan Fang 1 , Zhexiong Lian 2 , Yanmei Li 3 , Ruqi Tang 1 , Thomas Helleday 4 , M Eric Gershwin 5 , Zhengrui You 1 , Xiong Ma 1
|
Background & Aims
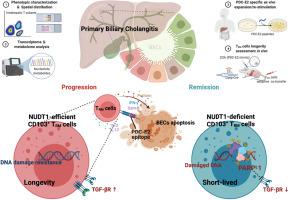
Pyruvate dehydrogenase (PDC)-E2 specific CD8+ T cells play a leading role in biliary destruction in PBC. However, there are limited data on the characterization of these autoantigen-specific CD8+ T cells, particularly in the liver. Herein, we aimed to identify pathogenic intrahepatic CD8+ T-cell subpopulations and investigate their immunobiology in PBC.
Methods
Phenotypic and functional analysis of intrahepatic T-cell subsets were performed by flow cytometry. CD103+ TRM cell frequency was evaluated by histological staining. The transcriptome and metabolome were analyzed by RNA-seq and liquid chromatography-mass spectrometry, respectively. Cytotoxicity of TRM cells against cholangiocytes was assayed in a 3D organoid co-culture system. Moreover, the longevity (long-term survival) of TRM cells in vivo was studied by 2-octynoic acid-BSA (2OA-BSA) immunization, Nudt1 conditional knock-out and adoptive co-transfer in a murine model.
Results
Intrahepatic CD103+ TRM (CD69+CD103+CD8+) cells were significantly expanded, hyperactivated, and potentially specifically reactive to PDC-E2 in patients with PBC. CD103+ TRM cell frequencies correlated with clinical and histological indices of PBC and predicted poor ursodeoxycholic acid response. NUDT1 blockade suppressed the cytotoxic effector functions of CD103+ TRM cells upon PDC-E2 re-stimulation. NUDT1 overexpression in CD8+ T cells promoted tissue-residence programming in vitro; inhibition or knockdown of NUDT1 had the opposite effect. Pharmacological blockade or genetic deletion of NUDT1 eliminated CD103+ TRM cells and alleviated cholangitis in mice immunized with 2OA-BSA. Significantly, NUDT1-dependent DNA damage resistance potentiates CD8+ T-cell tissue-residency via the PARP1-TGFβR axis in vitro. Consistently, PARP1 inhibition restored NUDT1-deficient CD103+ TRM cell durable survival and TGFβ-Smad signaling.
Conclusions
CD103+ TRM cells are the dominant population of PDC-E2-specific CD8+ T lymphocytes in the livers of patients with PBC. The role of NUDT1 in promoting pathogenic CD103+ TRM cell accumulation and longevity represents a novel therapeutic target in PBC.
Lay summary
Primary biliary cholangitis (PBC) is a rare inflammatory condition of the bile ducts. It can be treated with ursodeoxycholic acid, but a large percentage of patients respond poorly to this treatment. Liver-infiltrating memory CD8+ T cells recognizing the PDC-E2 immunodominant epitope are critical in the pathogenesis of PBC. We identifed the key pathogenic CD8+ T cell subset, and worked out the mechanisms of its hyperactivation and longevity, which could be exploited therapeutically.
中文翻译:

NUDT1促进原发性胆汁性胆管炎中CD103+ TRM细胞的积累和寿命
背景与目标
丙酮酸脱氢酶 (PDC)-E2 特异性 CD8 + T 细胞在 PBC 的胆道破坏中起主导作用。然而,关于这些自身抗原特异性 CD8 + T 细胞特征的数据有限,特别是在肝脏中。在此,我们旨在鉴定致病性肝内 CD8 + T 细胞亚群并研究它们在 PBC 中的免疫生物学。
方法
通过流式细胞术对肝内 T 细胞亚群进行表型和功能分析。通过组织学染色评估CD103 + T RM细胞频率。转录组和代谢组分别通过 RNA-seq 和液相色谱-质谱法进行分析。在 3D 类器官共培养系统中测定了T RM细胞对胆管细胞的细胞毒性。此外,通过小鼠模型中的 2-辛酸-BSA (2OA-BSA) 免疫、Nudt1条件性敲除和过继性共转移研究了 T RM细胞在体内的寿命(长期存活) 。
结果
在 PBC 患者中,肝内 CD103 + T RM (CD69 + CD103 + CD8 + ) 细胞显着扩增、过度活化,并可能对 PDC-E2 产生特异性反应。CD103 + T RM细胞频率与 PBC 的临床和组织学指标相关,并预测熊去氧胆酸反应不良。NUDT1 阻断抑制了 CD103 + T RM细胞在 PDC-E2 再刺激后的细胞毒性效应功能。CD8 + T细胞中的NUDT1过表达促进了体外组织驻留编程; NUDT1的抑制或敲低具有相反的效果。NUDT1 的药理学阻断或基因缺失消除了 CD103 + T RM细胞并减轻了用 2OA-BSA 免疫的小鼠的胆管炎。值得注意的是,NUDT1 依赖性 DNA 损伤抗性通过体外PARP1-TGFβR 轴增强 CD8 + T 细胞组织驻留。一致地,PARP1 抑制恢复了 NUDT1 缺陷型 CD103 + T RM细胞的持久存活和 TGFβ - Smad 信号传导。
结论
CD103 + T RM细胞是PBC 患者肝脏中PDC-E2 特异性 CD8 + T 淋巴细胞的主要群体。NUDT1 在促进致病性 CD103 + T RM细胞积累和长寿中的作用代表了 PBC 的新治疗靶点。
总结
原发性胆汁性胆管炎 (PBC) 是一种罕见的胆管炎症性疾病。它可以用熊去氧胆酸治疗,但大部分患者对这种治疗反应不佳。识别 PDC-E2 免疫显性表位的肝浸润记忆 CD8 + T 细胞在 PBC 的发病机制中至关重要。我们确定了关键的致病性 CD8 + T 细胞亚群,并研究了其过度活化和长寿的机制,可以在治疗上加以利用。











































 京公网安备 11010802027423号
京公网安备 11010802027423号