American Journal of Kidney Diseases ( IF 9.4 ) Pub Date : 2022-06-09 , DOI: 10.1053/j.ajkd.2022.04.009 Aleksandar Senev 1 , Elisabet Van Loon 2 , Evelyne Lerut 3 , Maarten Coemans 2 , Jasper Callemeyn 2 , Liesbeth Daniëls 4 , Johan Kerkhofs 4 , Priyanka Koshy 3 , Dirk Kuypers 5 , Baptiste Lamarthée 2 , Ben Sprangers 5 , Claire Tinel 2 , Amaryllis H Van Craenenbroeck 5 , Vicky Van Sandt 4 , Marie-Paule Emonds 1 , Maarten Naesens 5
|
Rationale & Objective
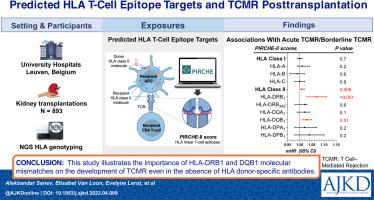
The relationship between human leukocyte antigen (HLA) molecular mismatches and T-cell–mediated rejection (TCMR) is unknown. We investigated the associations between the different donor HLA–derived T-cell targets and the occurrence of TCMR and borderline histologic changes suggestive of TCMR after kidney transplantation.
Study Design
Retrospective cohort study.
Setting & Participants
All kidney transplant recipients at a single center between 2004 and 2013 with available biopsy data and a DNA sample for high-resolution HLA donor/recipient typing (N = 893).
Exposure
Scores calculated by the HLA matching algorithm PIRCHE-II and HLA eplet mismatches.
Outcome
TCMR, borderline changes suggestive of TCMR, and allograft failure.
Analytical Approach
Multivariable cause-specific hazards models were fit to characterize the association between HLA epitopes targets and study outcomes.
Results
We found 277 patients developed TCMR, and 134 developed only borderline changes suggestive of TCMR on at least 1 biopsy. In multivariable analyses, only the PIRCHE-II scores for HLA-DRB1 and HLA-DQB1 were independently associated with the occurrence of TCMR and with allograft failure; this was not the case for HLA class I molecules. If restricted to rejection episodes within the first 3 months after transplantation, only the T-cell epitope targets originating from the donor’s HLA-DRB1 and HLA-DQB1, but not class I molecules, were associated with the early acute TCMR. Also, the median PIRCHE-II score for HLA class II was statistically different between the patients with TCMR compared to the patients without TCMR (129 [IQR, 60-240] vs 201 [IQR, 96-298], respectively; P < 0.0001). These differences were not observed for class I PIRCHE-II scores.
Limitations
Observational clinical data and residual confounding.
Conclusions
In the absence of HLA-DSA, HLA class II but not class I mismatches are associated with early episodes of acute TCMR and allograft failure. This suggests that current immunosuppressive therapies are largely able to abort the most deleterious HLA class I–directed alloimmune processes; however, alloresponses against HLA-DRB1 and HLA-DQB1 molecular mismatches remain insufficiently suppressed.
Plain-Language Summary
Genetic differences in the human leukocyte antigen (HLA) complex between kidney transplant donors and recipients play a central role in T-cell–mediated rejection (TCMR), which can lead to failure of the transplanted kidney. Evaluating this genetic disparity (mismatch) in the HLA complex at the molecular (epitope) level could contribute to better prediction of the immune response to the donor organ posttransplantation. We investigated the associations of the different donor HLA–derived T-cell epitope targets and scores obtained from virtual crossmatch algorithms with the occurrence of TCMR, borderline TCMR, and graft failure after kidney transplantation after taking into account the influence of donor-specific anti-HLA antibodies. This study illustrates the greater importance of the molecular mismatches in class II molecules compared to class I HLA molecules.
中文翻译:

预测的 HLA T 细胞表位靶标与肾移植后 T 细胞介导的排斥反应的关联
理由和目标
人类白细胞抗原 (HLA) 分子错配与 T 细胞介导的排斥反应 (TCMR) 之间的关系尚不清楚。我们研究了不同供体 HLA 来源的 T 细胞靶标与 TCMR 的发生以及肾移植后提示 TCMR 的临界组织学变化之间的关联。
学习规划
回顾性队列研究。
设置和参与者
2004 年至 2013 年间在一个中心的所有肾移植受者,具有可用的活检数据和用于高分辨率 HLA 供体/受体分型的 DNA 样本(N = 893)。
接触
通过 HLA 匹配算法 PIRCHE-II 和 HLA eplet 不匹配计算的分数。
结果
TCMR、提示 TCMR 的临界变化和同种异体移植物失败。
分析方法
多变量特定原因危害模型适合描述 HLA 表位目标与研究结果之间的关联。
结果
我们发现 277 名患者出现了 TCMR,而 134 名患者至少在 1 次活检中仅出现提示 TCMR 的临界变化。在多变量分析中,只有 HLA-DRB1 和 HLA-DQB1 的 PIRCHE-II 评分与 TCMR 的发生和同种异体移植失败独立相关;HLA I 类分子的情况并非如此。如果仅限于移植后前 3 个月内的排斥反应,只有来自供体 HLA-DRB1 和 HLA-DQB1 的 T 细胞表位靶标与早期急性 TCMR 相关,而 I 类分子则没有。此外,与没有 TCMR 的患者相比,具有 TCMR 的患者的 HLA II 类 PIRCHE-II 评分中位数有统计学差异(分别为 129 [IQR,60-240] 和 201 [IQR,96-298];P < 0.0001)。I 类 PIRCHE-II 分数没有观察到这些差异。
限制
观察性临床数据和残余混杂。
结论
在没有 HLA-DSA 的情况下,HLA II 类而非 I 类错配与急性 TCMR 和同种异体移植失败的早期发作相关。这表明目前的免疫抑制疗法在很大程度上能够中止最有害的 HLA I 类定向同种免疫过程;然而,针对 HLA-DRB1 和 HLA-DQB1 分子错配的同种异体反应仍未得到充分抑制。
通俗易懂的摘要
肾移植供体和受体之间人类白细胞抗原 (HLA) 复合体的遗传差异在 T 细胞介导的排斥反应 (TCMR) 中起着核心作用,这可能导致移植肾的衰竭。在分子(表位)水平上评估 HLA 复合体中的这种遗传差异(错配)可能有助于更好地预测移植后对供体器官的免疫反应。在考虑了供体特异性抗- HLA 抗体。







































 京公网安备 11010802027423号
京公网安备 11010802027423号