The Journal of Thoracic and Cardiovascular Surgery ( IF 4.9 ) Pub Date : 2022-06-02 , DOI: 10.1016/j.jtcvs.2022.05.029 Andrew H Smith 1 , Andrew Y Shin 2 , Sarah Tabbutt 3 , Mousumi Banerjee 4 , Wenying Zhang 4 , Santiago Borasino 5 , Justin J Elhoff 6 , J William Gaynor 7 , Nancy S Ghanayem 8 , Sara K Pasquali 9 , James D St Louis 10 , Subhadra Shashidharan 11 , Michael Ruppe 12 , Kurt R Schumacher 9 , Michael Gaies 9 , John M Costello 13
|
Objective
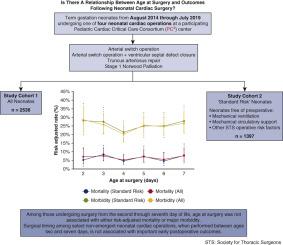
The optimal timing for neonatal cardiac surgery is a potentially modifiable factor that may affect outcomes. We studied the relationship between age at surgery (AAS) and outcomes across multiple hospitals, focusing on neonatal operations where timing appears is not emergency.
Methods
We studied neonates ≥37 weeks' gestation and ≥2.5 kg admitted to a treating hospital on or before day of life 2 undergoing selected index cardiac operations. The impact of AAS on outcomes was evaluated across the entire cohort and a standard risk subgroup (ie, free of preoperative mechanical ventilation, mechanical circulatory support, or other organ failure). Outcomes included mortality, major morbidity (ie, cardiac arrest, mechanical circulatory support, unplanned cardiac reintervention, or neurologic complication), and postoperative cardiac intensive care unit and hospital length of stay. Post hoc analyses focused on operations undertaken between day of life 2 and 7.
Results
We studied 2536 neonates from 47 hospitals. AAS from day of life 2 through 7 was not associated with risk adjusted mortality or major morbidity among the entire cohort and the standard risk subgroup. Older AAS, although associated with modest increases in postoperative cardiac intensive care unit and hospital length of stay in the entire cohort, was not associated with hospital length of stay in the standard risk subgroup.
Conclusions
Among select nonemergency neonatal cardiac operations, AAS between day of life 2 and 7 was not found to be associated with risk adjusted mortality or major morbidity. Although delays in surgical timing may modestly increase preoperative resource use, studies of AAS and outcomes not evident at the time of discharge are needed.
中文翻译:

手术年龄和新生儿心脏手术后的结果:来自儿科心脏重症监护协会的分析
客观的
新生儿心脏手术的最佳时机是一个可能影响结果的潜在可变因素。我们研究了多家医院的手术年龄 (AAS) 与结果之间的关系,重点关注出现时机并非紧急情况的新生儿手术。
方法
我们研究了妊娠 ≥ 37 周且体重 ≥ 2.5 kg 的新生儿在出生后第 2 天或之前入院接受选定的心脏手术。AAS 对结果的影响在整个队列和标准风险亚组(即,无术前机械通气、机械循环支持或其他器官衰竭)中进行了评估。结果包括死亡率、主要发病率(即心脏骤停、机械循环支持、计划外心脏再介入或神经系统并发症),以及术后心脏重症监护病房和住院时间。事后分析侧重于生命第 2 天和第 7 天之间进行的操作。
结果
我们研究了来自 47 家医院的 2536 名新生儿。从出生第 2 天到第 7 天的 AAS 与整个队列和标准风险亚组的风险调整死亡率或主要发病率无关。较年长的 AAS,虽然与术后心脏重症监护病房和整个队列住院时间的适度增加有关,但与标准风险亚组的住院时间无关。
结论
在选定的非紧急新生儿心脏手术中,未发现出生后第 2 天至第 7 天的 AAS 与风险调整死亡率或主要发病率相关。虽然延迟手术时间可能会适度增加术前资源的使用,但需要对 AAS 和出院时不明显的结果进行研究。











































 京公网安备 11010802027423号
京公网安备 11010802027423号