Journal of Hepatology ( IF 26.8 ) Pub Date : 2022-05-31 , DOI: 10.1016/j.jhep.2022.05.021 Càndid Villanueva 1 , Ferran Torres 2 , Shiv Kumar Sarin 3 , Hasnain Ali Shah 4 , Dhiraj Tripathi 5 , Anna Brujats 6 , Susana G Rodrigues 7 , Ankit Bhardwaj 8 , Zahid Azam 9 , Peter C Hayes 10 , Ankur Jindal 3 , Shahab Abid 4 , Edilmar Alvarado 1 , Jaume Bosch 11 ,
|
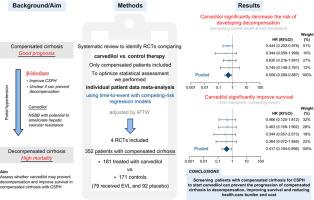
Background & Aims
Whether non-selective β-blockers can prevent decompensation of cirrhosis warrants clarification. Carvedilol might be particularly effective since its intrinsic vasodilatory activity may ameliorate hepatic vascular resistance, a major mechanism of portal hypertension in early cirrhosis. We assessed whether carvedilol may prevent decompensation and improve survival in patients with compensated cirrhosis and clinically significant portal hypertension (CSPH).
Methods
By systematic review we identified randomized-controlled trials (RCTs) comparing carvedilol vs. control therapy (no-active treatment or endoscopic variceal ligation [EVL]) in patients with cirrhosis and CSPH without previous bleeding. We performed a competing-risk time-to-event meta-analysis using individual patient data (IPD) obtained from principal investigators of RCTs. Only compensated patients were included. Primary outcomes were prevention of decompensation (liver transplantation and death were competing events) and death (liver transplantation was a competing event). Models were adjusted using propensity scores for baseline covariates with the inverse probability of treatment weighting (IPTW) approach.
Results
Among 125 full-text studies evaluated, 4 RCTs were eligible. The 4 provided IPD and were included, comprising 352 patients with compensated cirrhosis, 181 treated with carvedilol and 171 controls (79 received EVL and 92 placebo). Baseline characteristics were similar between groups. Standardized differences were <10% by IPTW. The risk of developing decompensation of cirrhosis was lower with carvedilol than in controls (subdistribution hazard ratio [SHR] 0.506; 95% CI 0.289-0.887; p = 0.017; I2 = 0.0%, Q-statistic-p = 0.880), mainly due to a reduced risk of ascites (SHR 0.491; 95% CI 0.247-0.974; p = 0.042; I2 = 0.0%, Q-statistic-p = 0.384). The risk of death was also lower with carvedilol (SHR 0.417; 95% CI 0.194-0.896; p = 0.025; I2 = 0.0%, Q-statistic-p = 0.989).
Conclusions
Long-term carvedilol therapy reduced decompensation of cirrhosis and significantly improved survival in compensated patients with CSPH. This suggests that screening patients with compensated cirrhosis for CSPH to enable the prompt initiation of carvedilol could improve outcomes.
PROSPERO registration number
CRD42019144786.
Lay summary
The transition from compensated cirrhosis to decompensated cirrhosis is associated with markedly reduced life expectancy. Therefore, preventing decompensation in patients with compensated cirrhosis would be associated with greatly improved patient outcomes. There has been controversy regarding the use of non-selective β-blockers (portal pressure-lowering medications) in patients with cirrhosis and elevated portal blood pressure (portal hypertension). Herein, using a competing-risk meta-analysis to optimize sample size and properly investigate cirrhosis as a multistate disease and outcomes as time-dependent events, we show that carvedilol (a non-selective β-blocker) is associated with a reduced risk of decompensating events and improved survival in patients with cirrhosis and portal hypertension.
中文翻译:

在一项竞争风险荟萃分析中,卡维地洛可降低代偿性肝硬化患者失代偿和死亡的风险
背景与目标
非选择性β受体阻滞剂是否可以预防肝硬化失代偿值得澄清。卡维地洛可能特别有效,因为其内在的血管舒张活性可以改善肝血管阻力,这是早期肝硬化门静脉高压的主要机制。我们评估了卡维地洛是否可以预防代偿性肝硬化和有临床意义的门脉高压(CSPH)患者的失代偿并提高生存率。
方法
通过系统评价,我们确定了比较卡维地洛与卡维地洛的随机对照试验 (RCT)。对既往无出血的肝硬化和 CSPH 患者进行对照治疗(非积极治疗或内镜下静脉曲张结扎术 [EVL])。我们使用从随机对照试验主要研究人员获得的个体患者数据(IPD)进行了竞争风险事件时间荟萃分析。仅包括补偿患者。主要结局是预防失代偿(肝移植和死亡是竞争事件)和死亡(肝移植是竞争事件)。使用基线协变量的倾向评分和治疗加权逆概率(IPTW)方法对模型进行调整。
结果
在评估的 125 项全文研究中,有 4 项随机对照试验合格。 4 名提供 IPD 的患者被纳入其中,其中包括 352 名代偿性肝硬化患者、181 名接受卡维地洛治疗的患者和 171 名对照患者(79 名接受 EVL 治疗,92 名接受安慰剂)。各组之间的基线特征相似。标准化差异为<10 id=13>p = 0.017; I 2 = 0.0%,Q-统计- p = 0.880),主要是由于腹水风险降低(SHR 0.491;95% CI 0.247-0.974; p = 0.042;I 2 = 0.0%,Q-统计- p = 0.384)。卡维地洛的死亡风险也较低(SHR 0.417;95% CI 0.194-0.896; p = 0.025;I 2 = 0.0%,Q 统计量 - p = 0.989)。
结论
长期卡维地洛治疗可减少肝硬化失代偿,并显着提高代偿性 CSPH 患者的生存率。这表明对代偿性肝硬化患者进行 CSPH 筛查以立即开始使用卡维地洛可以改善预后。
普洛斯彼罗注册号
CRD42019144786。
外行总结
从代偿性肝硬化到失代偿性肝硬化的转变与预期寿命的显着缩短有关。因此,预防代偿性肝硬化患者的失代偿将大大改善患者的预后。对于肝硬化和门静脉血压升高(门静脉高压)患者使用非选择性β受体阻滞剂(门静脉压降低药物)一直存在争议。在此,使用竞争风险荟萃分析来优化样本量并正确研究肝硬化作为一种多态疾病和作为时间依赖性事件的结果,我们表明卡维地洛(一种非选择性β受体阻滞剂)与降低肝硬化风险相关肝硬化和门静脉高压患者的失代偿事件并提高生存率。











































 京公网安备 11010802027423号
京公网安备 11010802027423号