JACC: Cardiovascular Imaging ( IF 12.8 ) Pub Date : 2022-05-11 , DOI: 10.1016/j.jcmg.2022.03.024 Nicola Riccardo Pugliese 1 , Alessio Balletti 1 , Silvia Armenia 1 , Nicolò De Biase 1 , Francesco Faita 2 , Alessandro Mengozzi 1 , Francesco Paneni 3 , Frank Ruschitzka 3 , Agostino Virdis 1 , Lorenzo Ghiadoni 1 , Stefano Taddei 1 , Bryan Williams 4 , Francesco Antonini-Canterin 5 , Stefano Masi 6
|
Background
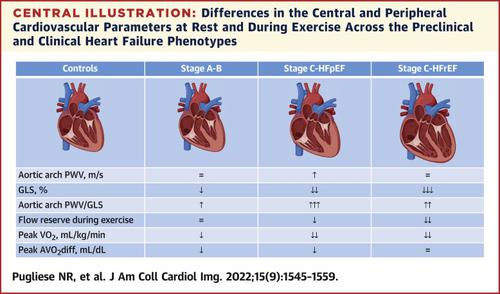
Ventricular-arterial coupling (VAC) can be evaluated as the ratio between arterial stiffness (pulsed wave velocity [PWV]) and myocardial deformation (global longitudinal strain [GLS]).
Objectives
This study aimed to evaluate VAC across the spectrum of heart failure (HF).
Methods
The authors introduced a Doppler-derived, single-beat technique to estimate aortic arch PWV (aa-PWV) in addition to tonometry-derived carotid-femoral PWV (cf-PWV). They measured PWVs and GLS in 155 healthy controls, 75 subjects at risk of developing HF (American College of Cardiology/American Heart Association stage A-B) and 236 patients in stage C heart failure with preserved ejection fraction (HFpEF) (n = 104) or heart failure with reduced ejection fraction (HFrEF) (n = 132). They evaluated peak oxygen consumption and peripheral extraction using combined cardiopulmonary-echocardiography exercise stress.
Results
aa-PWV was obtainable in all subjects and significantly lower than cf-PWV in all subgroups (P < 0.01). PWVs were directly related and increased with age (all P < 0.0001). cf-PWV/GLS was similarly compromised in HFrEF (1.09 ± 0.35) and HFpEF (1.05 ± 0.21), whereas aa-PWV/GLS was more impaired in HFpEF (0.70 ± 0.10) than HFrEF (0.61 ± 0.14; P < 0.01). Stage A-B had values of cf-PWV/GLS and aa-PWV/GLS (0.67 ± 0.27 and 0.48 ± 0.14, respectively) higher than controls (0.46 ± 0.11 and 0.39 ± 0.10, respectively) but lower than stage C (all P < 0.01). Peak arteriovenous oxygen difference (AVO2diff) was inversely related with cf-PWV/GLS and aa-PWV/GLS (all P < 0.01). Although cf-PWV/GLS and aa-PWV/GLS independently predicted peak VO2 in the overall population (adjusted R2 = 0.33 and R2= 0.36; all P < 0.0001), only aa-PWV/GLS was independently associated with flow reserve during exercise (R2 = 0.52; P < 0.0001).
Conclusions
Abnormal VAC is directly correlated with greater severity of HF and worse functional capacity. HFpEF shows a worse VAC than HFrEF when expressed by aa-PWV/GLS.
中文翻译:

心力衰竭谱中近端主动脉僵硬度和有氧能力的心室-动脉耦合
背景
心室-动脉耦合 (VAC) 可以评估为动脉硬度 (脉冲波速度 [PWV]) 和心肌变形 (全局纵向应变 [GLS]) 之间的比率。
目标
本研究旨在评估心力衰竭 (HF) 范围内的 VAC。
方法
除了眼压计衍生的颈股动脉 PWV (cf-PWV) 之外,作者还介绍了一种多普勒衍生的单次搏动技术来估计主动脉弓 PWV (aa-PWV)。他们测量了 155 名健康对照、75 名有心衰风险的受试者(美国心脏病学会/美国心脏协会 AB 期)和 236 名 C 期射血分数保留 (HFpEF) 心力衰竭患者(n = 104)或射血分数降低的心力衰竭 (HFrEF) (n = 132)。他们使用联合心肺超声心动图运动压力评估了峰值耗氧量和外周抽吸。
结果
所有受试者均获得 aa-PWV,并且在所有亚组中均显着低于 cf-PWV(P < 0.01)。PWV 与年龄直接相关并随着年龄的增长而增加(所有P < 0.0001)。cf-PWV/GLS 在 HFrEF (1.09 ± 0.35) 和 HFpEF (1.05 ± 0.21) 中同样受损,而在 HFpEF (0.70 ± 0.10) 中 aa-PWV/GLS 比 HFrEF (0.61 ± 0.14; P < 0.01)受损更严重. AB 期的 cf-PWV/GLS 和 aa-PWV/GLS 值(分别为 0.67 ± 0.27 和 0.48 ± 0.14)高于对照组(分别为 0.46 ± 0.11 和 0.39 ± 0.10)但低于 C 期(所有P < 0.01)。峰值动静脉血氧差(AVO 2 diff)与 cf-PWV/GLS 和 aa-PWV/GLS 呈负相关(所有P <0.01)。尽管 cf-PWV/GLS 和 aa-PWV/GLS 独立预测了总体人群中的峰值 VO 2 (调整后的 R 2 = 0.33 和 R 2 = 0.36;所有P < 0.0001),但只有 aa-PWV/GLS 与流量独立相关运动期间的储备(R 2 = 0.52;P < 0.0001)。
结论
VAC 异常与 HF 的更严重程度和更差的功能能力直接相关。当用 aa-PWV/GLS 表示时,HFpEF 显示出比 HFrEF 更差的 VAC。











































 京公网安备 11010802027423号
京公网安备 11010802027423号