JACC: Heart Failure ( IF 10.3 ) Pub Date : 2022-04-06 , DOI: 10.1016/j.jchf.2022.01.020 James P Curtain 1 , Ross T Campbell 1 , Mark C Petrie 1 , Alice M Jackson 1 , William T Abraham 2 , Akshay S Desai 3 , Kenneth Dickstein 4 , Lars Køber 5 , Jean L Rouleau 6 , Karl Swedberg 7 , Michael R Zile 8 , Scott D Solomon 3 , Pardeep S Jhund 1 , John J V McMurray 1
|
Background
Up to 20% of patients in heart failure with reduced ejection fraction (HFrEF) trials are not taking diuretic agents at baseline, but little is known about them.
Objectives
The aim of this study was to examine outcomes in patients with HFrEF not taking diuretic medications and after diuretic medications are started.
Methods
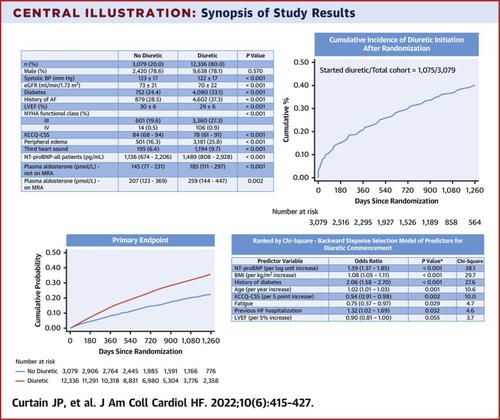
Patient characteristics and outcomes were compared between patients taking or not taking diuretic drugs at baseline in the ATMOSPHERE (Aliskiren Trial of Minimizing Outcomes for Patients With Heart Failure) and PARADIGM-HF (Prospective Comparison of ARNI With ACEI to Determine Impact on Global Mortality and Morbidity in Heart Failure Trial) trials combined. Patients starting diuretic medications were also compared with those remaining off diuretic drugs during follow-up. Symptoms (Kansas City Cardiomyopathy Questionnaire Clinical Summary Score [KCCQ-CSS]), hospitalization for worsening heart failure (HF), mortality, and kidney function (estimated glomerular filtration rate slope) were examined.
Results
At baseline, the 3,079 of 15,415 patients (20%) not taking diuretic medications had a less severe HF profile, less neurohumoral activation, and better kidney function. They were less likely to experience the primary outcome (hospitalization for HF or cardiovascular death) than patients taking diuretic agents (adjusted HR: 0.77; 95% CI: 0.74-0.80; P < 0.001) and death of any cause. Commencement of a diuretic drug was associated with higher subsequent risk for death (adjusted HR: 2.05; 95% CI: 1.99-2.11; P < 0.001) and greater decreases in KCCQ-CSS and estimated glomerular filtration rate. The 5 strongest predictors of initiation of diuretic medications were higher N-terminal pro–B-type natriuretic peptide, higher body mass index, older age, history of diabetes, and worse KCCQ-CSS. In PARADIGM-HF, fewer patients who were treated with sacubitril/valsartan commenced diuretic agents (OR: 0.72; 95% CI: 0.58-0.88; P = 0.002).
Conclusions
Patients with HFrEF not taking diuretic medications and those who remained off them had better outcomes than patients treated with diuretic agents or who commenced them.
中文翻译:

HFrEF 患者与背景利尿剂使用和新利尿剂启动相关的临床结果
背景
在射血分数降低 (HFrEF) 试验中,多达 20% 的患者在基线时未服用利尿剂,但对此知之甚少。
目标
本研究的目的是检查未服用利尿药物的 HFrEF 患者和开始使用利尿药物后的结局。
方法
在 ATMOSPHERE(Aliskiren Trial of Minimizing Outcomes for Patients With Failure)和 PARADIGM-HF(ARNI 与 ACEI 的前瞻性比较以确定对全球死亡率和发病率的影响)中比较基线时服用或未服用利尿药的患者特征和结果在心力衰竭试验中)试验相结合。还比较了开始服用利尿剂药物的患者与随访期间停用利尿剂药物的患者。检查症状(堪萨斯城心肌病问卷临床总结评分 [KCCQ-CSS])、因心力衰竭 (HF) 恶化而住院、死亡率和肾功能(估计的肾小球滤过率斜率)。
结果
在基线时,未服用利尿剂药物的 15,415 名患者中有 3,079 名 (20%) 的心衰情况较轻,神经体液激活较少,肾功能较好。与服用利尿剂的患者(调整后的 HR:0.77;95% CI:0.74-0.80;P < 0.001)和全因死亡相比,他们经历主要结局(因心衰或心血管死亡住院)的可能性更小。开始使用利尿剂与更高的后续死亡风险相关(调整后的 HR:2.05;95% CI:1.99-2.11;P <0.001) 以及 KCCQ-CSS 和估计肾小球滤过率的更大降低。开始使用利尿剂药物的 5 个最强预测因素是更高的 N 末端前 B 型钠尿肽、更高的体重指数、更高的年龄、糖尿病史和更差的 KCCQ-CSS。在 PARADIGM-HF 中,较少接受沙库巴曲/缬沙坦治疗的患者开始使用利尿剂(OR:0.72;95% CI:0.58-0.88;P = 0.002)。
结论
未服用利尿剂药物的 HFrEF 患者和那些没有服用利尿剂药物的患者比接受利尿剂治疗或开始使用利尿剂药物的患者有更好的结果。











































 京公网安备 11010802027423号
京公网安备 11010802027423号