Journal of Hepatology ( IF 26.8 ) Pub Date : 2021-12-03 , DOI: 10.1016/j.jhep.2021.11.025 Georg Semmler 1 , Elias Laurin Meyer 2 , Karin Kozbial 3 , Philipp Schwabl 1 , Stefanie Hametner-Schreil 4 , Alberto Zanetto 5 , David Bauer 1 , David Chromy 1 , Benedikt Simbrunner 1 , Bernhard Scheiner 1 , Albert F Stättermayer 1 , Matthias Pinter 1 , Rainer Schöfl 4 , Francesco Paolo Russo 5 , Helena Greenfield 6 , Michael Schwarz 7 , Caroline Schwarz 7 , Michael Gschwantler 7 , Sonia Alonso López 8 , Maria Luisa Manzano 9 , Adriana Ahumada 10 , Rafael Bañares 11 , Mònica Pons 12 , Sergio Rodríguez-Tajes 13 , Joan Genescà 14 , Sabela Lens 13 , Michael Trauner 3 , Peter Ferenci 3 , Thomas Reiberger 1 , Mattias Mandorfer 1
|
Background & Aims
Hepatocellular carcinoma (HCC) is a major cause of morbidity and mortality in patients with advanced chronic liver disease (ACLD) caused by chronic hepatitis C who have achieved sustained virologic response (SVR). We developed risk stratification algorithms for de novo HCC development after SVR and validated them in an independent cohort.
Methods
We evaluated the occurrence of de novo HCC in a derivation cohort of 527 patients with pre-treatment ACLD and SVR to interferon-free therapy, in whom alpha-fetoprotein (AFP) and non-invasive surrogates of portal hypertension including liver stiffness measurement (LSM) were assessed pre-/post-treatment. We validated our results in 1,500 patients with compensated ACLD (cACLD) from other European centers.
Results
During a median follow-up (FU) of 41 months, 22/475 patients with cACLD (4.6%, 1.45/100 patient-years) vs. 12/52 decompensated patients (23.1%, 7.00/100 patient-years, p <0.001) developed de novo HCC. Since decompensated patients were at substantial HCC risk, we focused on cACLD for all further analyses.
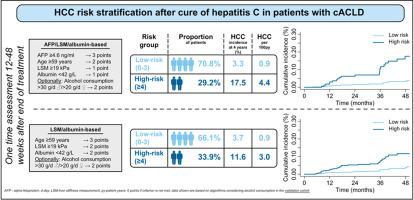
In cACLD, post-treatment-values showed a higher discriminative ability for patients with/without de novo HCC development during FU than pre-treatment values or absolute/relative changes. Models based on post-treatment AFP, alcohol consumption (optional), age, LSM, and albumin, accurately predicted de novo HCC development (bootstrapped Harrel’s C with/without considering alcohol: 0.893/0.836). Importantly, these parameters also provided independent prognostic information in competing risk analysis and accurately stratified patients into low- (~2/3 of patients) and high-risk (~1/3 of patients) groups in the derivation (algorithm with alcohol consumption; 4-year HCC-risk: 0% vs. 16.5%) and validation (3.3% vs. 17.5%) cohorts. An alternative approach based on alcohol consumption (optional), age, LSM, and albumin (i.e., without AFP) also showed a robust performance.
Conclusions
Simple algorithms based on post-treatment age/albumin/LSM, and optionally, AFP and alcohol consumption, accurately stratified patients with cACLD based on their risk of de novo HCC after SVR. Approximately two-thirds were identified as having an HCC risk <1%/year in both the derivation and validation cohort, thereby clearly falling below the cost-effectiveness threshold for HCC surveillance.
Lay summary
Simple algorithms based on age, alcohol consumption, results of blood tests (albumin and α-fetoprotein), as well as liver stiffness measurement after the end of hepatitis C treatment identify a large proportion (approximately two-thirds) of patients with advanced but still asymptomatic liver disease who are at very low risk (<1%/year) of liver cancer development, and thus, might not need to undergo 6-monthly liver ultrasound.
中文翻译:

代偿期晚期慢性肝病患者丙型肝炎治愈后HCC风险分层
背景与目标
肝细胞癌 (HCC) 是由慢性丙型肝炎引起的晚期慢性肝病 (ACLD) 患者发病率和死亡率的主要原因,这些患者已获得持续病毒学应答 (SVR)。我们开发了 SVR 后新发HCC 发展的风险分层算法,并在一个独立队列中对其进行了验证。
方法
我们评估了527 名接受无干扰素治疗前 ACLD 和 SVR 患者的衍生队列中新发 HCC 的发生,其中甲胎蛋白 (AFP) 和门静脉高压的非侵入性替代物,包括肝硬度测量 (LSM ) ) 在治疗前/治疗后进行评估。我们在来自其他欧洲中心的 1,500 名代偿性 ACLD (cACLD) 患者中验证了我们的结果。
结果
在 41 个月的中位随访 (FU) 中,22/475 名 cACLD 患者(4.6%,1.45/100 患者年)与12/52 名失代偿患者(23.1%,7.00/100 患者年,p < 0.001)从头开发HCC。由于失代偿患者存在相当大的 HCC 风险,我们将重点放在 cACLD 进行所有进一步分析。
在 cACLD 中,与治疗前值或绝对/相对变化相比,治疗后值对 FU 期间有/无新发 HCC 发展的患者具有更高的辨别能力。基于治疗后 AFP、酒精消耗量(可选)、年龄、LSM 和白蛋白的模型,准确预测了新发HCC 发展(有/无考虑酒精的自举 Harrel's C:0.893/0.836)。重要的是,这些参数还在竞争风险分析中提供了独立的预后信息,并在推导(酒精消耗算法; 4 年 HCC 风险:0%对16.5%)和验证(3.3%对17.5%) 队列。基于酒精消耗量(可选)、年龄、LSM 和白蛋白(即没有 AFP)的替代方法也显示出稳健的性能。
结论
基于治疗后年龄/白蛋白/LSM 的简单算法,以及可选的 AFP 和酒精消耗,根据SVR 后新发 HCC的风险对cACLD患者进行准确分层。在推导和验证队列中,大约三分之二的 HCC 风险被确定为 <1%/年,因此明显低于 HCC 监测的成本效益阈值。
总结
基于年龄、饮酒量、血液检测结果(白蛋白和甲胎蛋白)以及丙型肝炎治疗结束后肝脏硬度测量的简单算法可识别出很大一部分(约三分之二)晚期但仍无症状性肝病患肝癌的风险非常低(<1%/年),因此可能不需要每 6 个月进行一次肝脏超声检查。











































 京公网安备 11010802027423号
京公网安备 11010802027423号