International Journal of Cardiology ( IF 3.2 ) Pub Date : 2021-11-19 , DOI: 10.1016/j.ijcard.2021.11.046 Yuhei Goriki 1 , Goro Yoshioka 2 , Masahiro Natsuaki 2 , Kodai Shinzato 2 , Kensaku Nishihira 3 , Nehiro Kuriyama 3 , Mitsuhiro Shimomura 4 , Yohei Inoue 5 , Toshiyuki Nishikido 5 , Tetsuya Kaneko 2 , Kensuke Yokoi 2 , Ayumu Yajima 2 , Yoshiko Sakamoto 2 , Motoko Tago 2 , Atsushi Kawaguchi 6 , Fumi Yamamoto 7 , Atsushi Tanaka 2 , Takanori Yamaguchi 2 , Aya Shiraki 2 , Machiko Asaka 2 , Norihiko Kotooka 2 , Shinjo Sonoda 2 , Yutaka Hikichi 5 , Yoshisato Shibata 3 , Koichi Node 2
|
Background
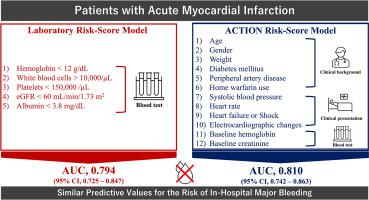
In-hospital bleeding is associated with poor prognosis in patients with acute myocardial infarction (AMI). We sought to investigate whether a combination of pre-procedural blood tests could predict the incidence of in-hospital major bleeding in patients with AMI.
Methods and results
A total of 1684 consecutive AMI patients who underwent primary percutaneous coronary intervention (PCI) were recruited and randomly divided into derivation (n = 1010) and validation (n = 674) cohorts. A risk-score model was created based on a combination of parameters assessed on routine blood tests on admission. In the derivation cohort, multivariate analysis revealed that the following 5 variables were significantly associated with in-hospital major bleeding: hemoglobin level < 12 g/dL (odds ratio [OR], 3.32), white blood cell count >10,000/μL (OR, 2.58), platelet count <150,000/μL (OR, 2.51), albumin level < 3.8 mg/dL (OR, 2.51), and estimated glomerular filtration rate < 60 mL/min/1.73 m2 (OR, 2.31). Zero to five points were given according to the number of these factors each patient had. Incremental risk scores were significantly associated with a higher incidence of in-hospital major bleeding in both cohorts (P < 0.001). Receiver operating characteristic curve analysis of risk models showed adequate discrimination between patients with and without in-hospital major bleeding (derivation cohort: area under the curve [AUC], 0.807; 95% confidence interval [CI], 0.759–0.848; validation cohort: AUC, 0.793; 95% CI, 0.725–0.847).
Conclusions
Our novel laboratory-based bleeding risk model could be useful for simple and objective prediction of in-hospital major bleeding events in patients with AMI.
中文翻译:

基于多种血液变量的急性心肌梗死患者院内大出血的简单风险评分模型
背景
院内出血与急性心肌梗死 (AMI) 患者的不良预后相关。我们试图调查术前血液检查的组合是否可以预测 AMI 患者院内大出血的发生率。
方法和结果
共招募了 1684 名连续接受经皮冠状动脉介入治疗 (PCI) 的 AMI 患者,并随机分为推导 ( n = 1010) 和验证 ( n = 674) 队列。风险评分模型是根据入院时常规血液检查评估的参数组合创建的。在推导队列中,多变量分析显示以下 5 个变量与院内大出血显着相关:血红蛋白水平 < 12 g/dL(优势比 [OR],3.32),白细胞计数 >10,000/μL(OR , 2.58),血小板计数 <150,000/μL (OR, 2.51),白蛋白水平 < 3.8 mg/dL (OR, 2.51),估计肾小球滤过率 < 60 mL/min/1.73 m 2(或,2.31)。根据每位患者所具有的这些因素的数量,给予 0 到 5 分。在两个队列中,增加的风险评分与较高的院内大出血发生率显着相关(P < 0.001)。风险模型的接受者操作特征曲线分析显示有和没有院内大出血的患者之间有足够的区别(推导队列:曲线下面积 [AUC],0.807;95% 置信区间 [CI],0.759–0.848;验证队列: AUC,0.793;95% CI,0.725–0.847)。
结论
我们基于实验室的新型出血风险模型可用于简单客观地预测 AMI 患者的院内大出血事件。











































 京公网安备 11010802027423号
京公网安备 11010802027423号