JACC: Cardiovascular Interventions ( IF 11.7 ) Pub Date : 2021-11-10 , DOI: 10.1016/j.jcin.2021.08.024 Agam Bansal 1 , Ankur Kalra 1 , Anirudh Kumar 1 , Joseph Campbell 1 , Amar Krishnaswamy 1 , Samir R Kapadia 1 , Grant W Reed 1
|
Objectives
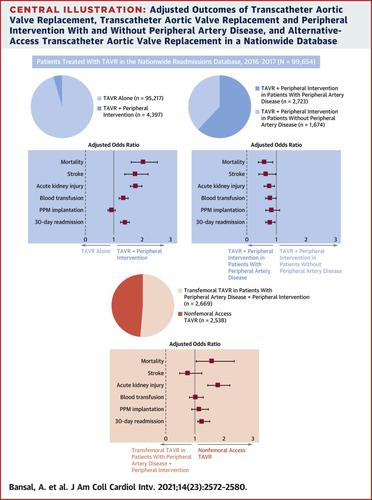
The aim of this study was to compare the prevalence and real-world outcomes of patients who require peripheral vascular intervention during the same hospitalization as transcatheter aortic valve replacement (TAVR) compared with TAVR alone.
Background
There are limited data on the prevalence and outcomes of combined TAVR and percutaneous peripheral vascular intervention.
Methods
All patients who underwent TAVR in 2016 and 2017 were identified using the Nationwide Readmissions Database. Outcomes of patients undergoing TAVR alone were compared with those of patients undergoing combined TAVR and peripheral intervention, TAVR and peripheral intervention with and without a history of peripheral artery disease, and alternative-access TAVR with transfemoral TAVR in individuals undergoing peripheral intervention. The primary outcome was in-hospital mortality.
Results
A total of 99,654 hospitalizations were identified, among which 4,397 patients (4.42%) underwent peripheral intervention during the same admission as TAVR. Patients who required peripheral intervention had increased mortality (4.2% vs 1.5%; P < 0.001), stroke (3.5% vs 1.8%; P < 0.001), acute kidney injury (17.6% vs 10.8%; P < 0.001), blood transfusion (16.0% vs 11.3%; P < 0.001), 30-day readmission (16.3% vs 12.1%; P < 0.001), median length of stay (4 days [IQR: 2-8 days] vs 3 days [IQR: 2-5 days]; P < 0.001), and hospitalization charges. Compared with patients undergoing peripheral intervention to facilitate transfemoral TAVR, alternative-access TAVR was associated with increased mortality (4.6% vs 3.0%; P = 0.036), acute kidney injury (22.7% vs 14.3%; P < 0.001), median length of stay (5 days [IQR: 3-10 days] vs 4 days [IQR: 2-7 days]; P < 0.001), and 30-day readmission (18.1% vs 15.5%; P = 0.012).
Conclusions
Peripheral vascular intervention may be used to facilitate transfemoral access or as a bailout for vascular complications during TAVR. Combined TAVR and peripheral intervention is associated with an increased risk for adverse events, though outcomes are better compared with alternative-access TAVR using a nonfemoral approach.
中文翻译:

美国联合经导管主动脉瓣置换术和外周血管介入治疗的结果
目标
本研究的目的是比较与单独的 TAVR 相比,在与经导管主动脉瓣置换术 (TAVR) 相同的住院期间需要外周血管干预的患者的患病率和真实世界结果。
背景
关于 TAVR 和经皮外周血管介入联合治疗的患病率和结果的数据有限。
方法
使用全国再入院数据库确定了 2016 年和 2017 年接受 TAVR 的所有患者。将单独接受 TAVR 的患者的结果与接受 TAVR 和外周干预联合治疗、有和没有外周动脉疾病病史的 TAVR 和外周介入治疗以及接受外周介入治疗的个体经股 TAVR 替代通路 TAVR 的结果进行比较。主要结局是住院死亡率。
结果
总共确定了 99,654 例住院治疗,其中 4,397 例(4.42%)患者在与 TAVR 同一入院期间接受了外周干预。需要外周干预的患者死亡率增加(4.2% vs 1.5%;P < 0.001)、中风(3.5% vs 1.8%;P < 0.001)、急性肾损伤(17.6% vs 10.8%;P < 0.001)、输血(16.0% vs 11.3%;P < 0.001),30 天再入院(16.3% vs 12.1%;P < 0.001),中位住院时间(4 天 [IQR:2-8 天] vs 3 天 [IQR:2 -5 天];P < 0.001) 和住院费用。与接受外周干预以促进经股动脉 TAVR 的患者相比,替代通路 TAVR 与死亡率增加(4.6% vs 3.0%;P = 0.036)、急性肾损伤(22.7% vs 14.3%;P < 0.001)、中位长度留(5 天 [IQR:3-10 天] vs 4 天 [IQR:2-7 天];P < 0.001)和 30 天再入院(18.1% vs 15.5%;P = 0.012)。
结论
外周血管介入可用于促进经股动脉通路或作为 TAVR 期间血管并发症的救助。TAVR 和外周干预相结合会增加不良事件的风险,但与使用非股动脉方法的替代通路 TAVR 相比,结果更好。











































 京公网安备 11010802027423号
京公网安备 11010802027423号