Clinical Gastroenterology and Hepatology ( IF 11.6 ) Pub Date : 2021-11-02 , DOI: 10.1016/j.cgh.2021.10.037 Louise Wang 1 , Frank I Scott 2 , Ben Boursi 3 , Kim A Reiss 4 , Sankey Williams 5 , Henry Glick 5 , Yu-Xiao Yang 6
|
Background & Aims
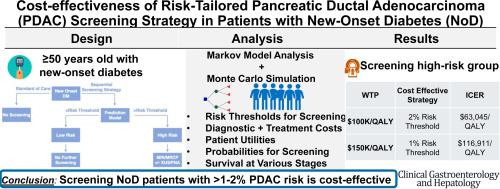
Screening for pancreatic ductal adenocarcinoma (PDAC) in asymptomatic adults is not recommended, however, patients with new-onset diabetes (NoD) have an 8 times higher risk of PDAC than expected. A novel risk-tailored early detection strategy targeting high-risk NoD patients might improve PDAC prognosis. We sought to evaluate the cost effectiveness of this strategy.
Methods
We compared PDAC early detection strategies targeting NoD individuals age 50 years and older at various minimal predicted PDAC risk thresholds vs standard of care in a Markov state–transition decision model under the health care sector perspective using a lifetime horizon.
Results
At a willingness to pay (WTP) threshold of $150,000 per quality-adjusted life-year, the early detection strategy targeting patients with a minimum predicted 3-year PDAC risk of 1% was cost effective (incremental cost-effectiveness ratio, $116,911). At a WTP threshold of $100,000 per quality-adjusted life-year, the early detection strategy at the 2% risk threshold was cost effective (incremental cost-effectiveness ratio, $63,045). The proportion of PDACs detected at local stage, costs of treatment for metastatic PDAC, utilities of local and regional cancers, and sensitivity of screening were the most influential parameters. Probabilistic sensitivity analysis confirmed that at a WTP threshold of $150,000, early detection at the 1.0% risk threshold was favored (30.6%), followed by the 0.5% risk threshold (20.4%) vs standard of care (1.7%). At a WTP threshold of $100,000, early detection at the 1.0% risk threshold was favored (27.3%) followed by the 2.0% risk threshold (22.8%) vs standard of care (2.0%).
Conclusions
A risk-tailored PDAC early detection strategy targeting NoD patients with a minimum predicted 3-year PDAC risk of 1.0% to 2.0% may be cost effective.
中文翻译:

针对新发糖尿病患者风险定制的胰腺癌早期检测策略的成本效益
背景与目标
不建议在无症状成人中筛查胰腺导管腺癌 (PDAC),但新发糖尿病 (NoD) 患者患 PDAC 的风险比预期高 8 倍。针对高风险 NoD 患者的新型风险定制早期检测策略可能会改善 PDAC 预后。我们试图评估该策略的成本效益。
方法
我们比较了针对 50 岁及以上 NoD 个体在各种最低预测 PDAC 风险阈值下的 PDAC 早期检测策略与医疗保健部门视角下的马尔可夫状态转变决策模型中的护理标准,使用生命周期。
结果
在每个质量调整生命年的支付意愿 (WTP) 阈值为 150,000 美元时,针对 3 年 PDAC 风险最低预测为 1% 的患者的早期检测策略具有成本效益(增量成本效益比为 116,911 美元)。在每个质量调整生命年的 WTP 阈值为 100,000 美元时,2% 风险阈值的早期检测策略具有成本效益(增量成本效益比为 63,045 美元)。局部阶段检测到的 PDAC 比例、转移性 PDAC 的治疗费用、局部和区域癌症的效用以及筛查的敏感性是最有影响力的参数。概率敏感性分析证实,在 WTP 阈值为 150,000 美元时,1.0% 风险阈值的早期检测受到青睐 (30.6%),其次是 0.5% 风险阈值 (20.4%) 与标准护理 (1.7%)。在 WTP 阈值为 100,000 美元时,1.0% 风险阈值的早期检测受到青睐 (27.3%),其次是 2.0% 风险阈值 (22.8%) 与标准护理 (2.0%)。
结论
针对 NoD 患者的风险定制 PDAC 早期检测策略(最低预测 3 年 PDAC 风险为 1.0% 至 2.0%)可能具有成本效益。











































 京公网安备 11010802027423号
京公网安备 11010802027423号