American Journal of Kidney Diseases ( IF 9.4 ) Pub Date : 2021-10-25 , DOI: 10.1053/j.ajkd.2021.09.008 Steven Menez 1 , Dennis G Moledina 2 , Heather Thiessen-Philbrook 1 , F Perry Wilson 2 , Wassim Obeid 1 , Michael Simonov 2 , Yu Yamamoto 2 , Celia P Corona-Villalobos 1 , Crystal Chang 1 , Brian T Garibaldi 3 , William Clarke 4 , Shelli Farhadian 5 , Charles Dela Cruz 6 , Steven G Coca 7 , Chirag R Parikh 1 ,
|
Rationale & Objective
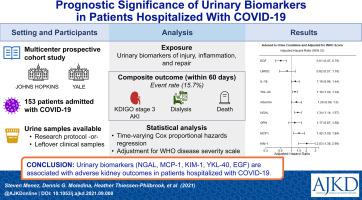
Acute kidney injury (AKI) is common in patients with coronavirus disease 2019 (COVID-19) and associated with poor outcomes. Urinary biomarkers have been associated with adverse kidney outcomes in other settings and may provide additional prognostic information in patients with COVID-19. We investigated the association between urinary biomarkers and adverse kidney outcomes among patients hospitalized with COVID-19.
Study Design
Prospective cohort study.
Setting & Participants
Patients hospitalized with COVID-19 (n = 153) at 2 academic medical centers between April and June 2020.
Exposure
19 urinary biomarkers of injury, inflammation, and repair.
Outcome
Composite of KDIGO (Kidney Disease: Improving Global Outcomes) stage 3 AKI, requirement for dialysis, or death within 60 days of hospital admission. We also compared various kidney biomarker levels in the setting of COVID-19 versus other common AKI settings.
Analytical Approach
Time-varying Cox proportional hazards regression to associate biomarker level with composite outcome.
Results
Out of 153 patients, 24 (15.7%) experienced the primary outcome. Twofold higher levels of neutrophil gelatinase-associated lipocalin (NGAL) (HR, 1.34 [95% CI, 1.14-1.57]), monocyte chemoattractant protein (MCP-1) (HR, 1.42 [95% CI, 1.09-1.84]), and kidney injury molecule 1 (KIM-1) (HR, 2.03 [95% CI, 1.38-2.99]) were associated with highest risk of sustaining primary composite outcome. Higher epidermal growth factor (EGF) levels were associated with a lower risk of the primary outcome (HR, 0.61 [95% CI, 0.47-0.79]). Individual biomarkers provided moderate discrimination and biomarker combinations improved discrimination for the primary outcome. The degree of kidney injury by biomarker level in COVID-19 was comparable to other settings of clinical AKI. There was evidence of subclinical AKI in COVID-19 patients based on elevated injury biomarker level in patients without clinical AKI defined by serum creatinine.
Limitations
Small sample size with low number of composite outcome events.
Conclusions
Urinary biomarkers are associated with adverse kidney outcomes in patients hospitalized with COVID-19 and may provide valuable information to monitor kidney disease progression and recovery.
中文翻译:

COVID-19 住院患者尿液生物标志物的预后意义
理由和目标
急性肾损伤 (AKI) 在 2019 年冠状病毒病 (COVID-19) 患者中很常见,并且与不良预后相关。尿液生物标志物在其他情况下与不良肾脏结局相关,并可能为 COVID-19 患者提供额外的预后信息。我们调查了 COVID-19 住院患者的尿液生物标志物与不良肾脏结局之间的关联。
研究设计
前瞻性队列研究。
背景及参与者
2020 年 4 月至 6 月期间在 2 个学术医疗中心住院的 COVID-19 患者 (n = 153)。
接触
19 种损伤、炎症和修复的尿液生物标志物。
结果
KDIGO(肾脏疾病:改善全球结果)3 期 AKI、需要透析或入院 60 天内死亡的复合材料。我们还比较了 COVID-19 背景下与其他常见 AKI 背景下的各种肾脏生物标志物水平。
分析法
时变 Cox 比例风险回归将生物标志物水平与复合结果相关联。
结果
在 153 名患者中,24 名 (15.7%) 经历了主要结局。中性粒细胞明胶酶相关脂质运载蛋白 (NGAL) (HR, 1.34 [95% CI, 1.14-1.57])、单核细胞趋化蛋白 (MCP-1) (HR, 1.42 [95% CI, 1.09-1.84]) 水平升高两倍,和肾损伤分子 1 (KIM-1)(HR,2.03 [95% CI,1.38-2.99])与维持主要复合结局的最高风险相关。表皮生长因子 (EGF) 水平较高与主要结局风险较低相关(HR,0.61 [95% CI,0.47-0.79])。单个生物标志物提供了适度的区分度,而生物标志物组合则改善了对主要结果的区分度。 COVID-19 中生物标志物水平的肾损伤程度与临床 AKI 的其他情况相当。根据血清肌酐定义的无临床 AKI 的患者损伤生物标志物水平升高,有证据表明 COVID-19 患者存在亚临床 AKI。
局限性
样本量小,复合结果事件数量少。
结论
尿液生物标志物与 COVID-19 住院患者的不良肾脏结局相关,可能为监测肾脏疾病进展和恢复提供有价值的信息。











































 京公网安备 11010802027423号
京公网安备 11010802027423号