Clinical Gastroenterology and Hepatology ( IF 11.6 ) Pub Date : 2021-10-07 , DOI: 10.1016/j.cgh.2021.09.041 Anneli Andersson 1 , Matt Kelly 1 , Kento Imajo 2 , Atsushi Nakajima 2 , Jonathan A Fallowfield 3 , Gideon Hirschfield 4 , Michael Pavlides 5 , Arun J Sanyal 6 , Mazen Noureddin 7 , Rajarshi Banerjee 1 , Andrea Dennis 1 , Stephen Harrison 8
|
Background & Aims
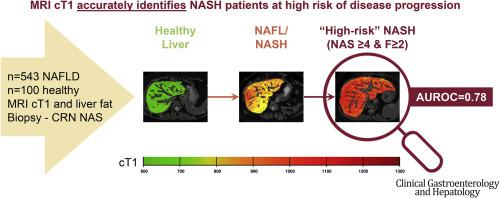
Nonalcoholic fatty liver disease (NAFLD) is increasing in prevalence worldwide. NAFLD is associated with excess risk of all-cause mortality, and its progression to nonalcoholic steatohepatitis (NASH) and fibrosis accounts for a growing proportion of cirrhosis and hepatocellular cancer and thus is a leading cause of liver transplant worldwide. Noninvasive precise methods to identify patients with NASH and NASH with significant disease activity and fibrosis are crucial when the disease is still modifiable. The aim of this study was to examine the clinical utility of corrected T1 (cT1) vs magnetic resonance imaging (MRI) liver fat for identification of NASH participants with nonalcoholic fatty liver disease activity score ≥4 and fibrosis stage (F) ≥2 (high-risk NASH).
Methods
Data from five clinical studies (n = 543) with participants suspected of NAFLD were pooled or used for individual participant data meta-analysis. The diagnostic accuracy of the MRI biomarkers to stratify NASH patients was determined using the area under the receiver operating characteristic curve (AUROC).
Results
A stepwise increase in cT1 and MRI liver fat with increased NAFLD severity was shown, and cT1 was significantly higher in participants with high-risk NASH. The diagnostic accuracy (AUROC) of cT1 to identify patients with NASH was 0.78 (95% CI, 0.74–0.82), for liver fat was 0.78 (95% CI, 0.73–0.82), and when combined with MRI liver fat was 0.82 (95% CI, 0.78–0.85). The diagnostic accuracy of cT1 to identify patients with high-risk NASH was good (AUROC = 0.78; 95% CI, 0.74–0.82), was superior to MRI liver fat (AUROC = 0.69; 95% CI, 0.64–0.74), and was not substantially improved by combining it with MRI liver fat (AUROC = 0.79; 95% CI, 0.75–0.83). The meta-analysis showed similar performance to the pooled analysis for these biomarkers.
Conclusions
This study shows that quantitative MRI-derived biomarkers cT1 and liver fat are suitable for identifying patients with NASH, and cT1 is a better noninvasive technology than liver fat to identify NASH patients at greatest risk of disease progression. Therefore, MRI cT1 and liver fat have important clinical utility to help guide the appropriate use of interventions in NAFLD and NASH clinical care pathways.
中文翻译:

磁共振成像生物标志物在识别具有高进展风险的非酒精性脂肪性肝炎患者中的临床应用:多中心汇总数据和荟萃分析
背景与目标
非酒精性脂肪性肝病 (NAFLD) 在全球范围内的患病率正在增加。NAFLD 与全因死亡风险过高有关,其进展为非酒精性脂肪性肝炎 (NASH) 和纤维化在肝硬化和肝细胞癌中的比例越来越高,因此是全球肝移植的主要原因。当疾病仍然可以改变时,无创精确方法来识别 NASH 和具有显着疾病活动和纤维化的 NASH 患者至关重要。本研究的目的是检查校正 T1 (cT1) 与磁共振成像 (MRI) 肝脏脂肪在识别非酒精性脂肪肝疾病活动评分≥4 和纤维化阶段 (F) ≥2 的 NASH 参与者(高-风险 NASH)。
方法
来自五项临床研究 (n = 543) 的疑似 NAFLD 参与者的数据被汇总或用于个体参与者数据荟萃分析。MRI 生物标志物对 NASH 患者进行分层的诊断准确性是使用受试者工作特征曲线下面积 (AUROC) 确定的。
结果
结果显示,随着 NAFLD 严重程度的增加,cT1 和 MRI 肝脏脂肪逐步增加,并且高危 NASH 参与者的 cT1 显着升高。cT1 识别 NASH 患者的诊断准确度 (AUROC) 为 0.78 (95% CI, 0.74–0.82),肝脏脂肪为 0.78 (95% CI, 0.73–0.82),结合 MRI 肝脏脂肪为 0.82 ( 95% CI,0.78–0.85)。cT1 对高危 NASH 患者的诊断准确性良好(AUROC = 0.78;95% CI,0.74-0.82),优于 MRI 肝脏脂肪(AUROC = 0.69;95% CI,0.64-0.74),并且将其与 MRI 肝脏脂肪相结合并没有显着改善(AUROC = 0.79;95% CI,0.75-0.83)。荟萃分析显示出与这些生物标志物的汇总分析相似的性能。
结论
本研究表明,定量 MRI 衍生的生物标志物 cT1 和肝脏脂肪适合识别 NASH 患者,而 cT1 是一种比肝脏脂肪更好的无创技术,可识别疾病进展风险最大的 NASH 患者。因此,MRI cT1 和肝脏脂肪具有重要的临床效用,可帮助指导在 NAFLD 和 NASH 临床护理途径中适当使用干预措施。











































 京公网安备 11010802027423号
京公网安备 11010802027423号