Chest ( IF 9.6 ) Pub Date : 2021-10-02 , DOI: 10.1016/j.chest.2021.09.032 Barry Burstein 1 , Sean van Diepen 2 , Brandon M Wiley 3 , Nandan S Anavekar 3 , Jacob C Jentzer 4
|
Background
Ventricular function, including left ventricular systolic dysfunction (LVSD), right ventricular systolic dysfunction (RVSD), and biventricular dysfunction (BVD), contribute to shock in cardiac ICU (CICU) patients, but the prognostic usefulness remains unclear.
Research Question
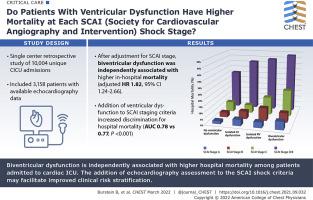
Do patients with ventricular dysfunction have higher mortality at each Society for Cardiovascular Angiography and Intervention (SCAI) shock stage?
Study Design and Methods
We identified patients in the CICU admitted with available echocardiography data. LVSD was defined as left ventricular ejection fraction < 40%, RVSD as moderate or greater systolic dysfunction by semiquantitative measurement, and BVD as the presence of both. Multivariate logistic regression determined the relationship between ventricular dysfunction and adjusted in-hospital mortality as a function of SCAI stage.
Results
The study population included 3,158 patients with a mean ± SD age of 68.2 ± 14.6 years, of which 51.8% had acute coronary syndromes. LVSD was present in 22.3%, RVSD in 11.8%, and BVD in 16.4%. After adjustment for SCAI shock stage, no difference in in-hospital mortality was found between patients with LVSD or RVSD and those without ventricular dysfunction (P > .05), but BVD was associated independently with higher in-hospital mortality (adjusted hazard ratio, 1.815; 95% CI, 1.237-2.663; P = .0023). The addition of ventricular dysfunction to the SCAI staging criteria increased discrimination for hospital mortality (area under the receiver operating characteristic curve, 0.784 vs 0.766; P < .001).
Interpretation
Among patients admitted to the CICU, only BVD was associated independently with higher hospital mortality. The addition of echocardiography assessment to the SCAI shock criteria may facilitate improved clinical risk stratification.
中文翻译:

双心室功能和休克严重程度预测心脏 ICU 患者的死亡率
背景
心室功能,包括左心室收缩功能障碍 (LVSD)、右心室收缩功能障碍 (RVSD) 和双心室功能障碍 (BVD),会导致心脏 ICU (CICU) 患者出现休克,但其预后价值仍不清楚。
研究问题
心室功能障碍患者在每个心血管血管造影和干预协会 (SCAI) 休克阶段的死亡率是否更高?
研究设计和方法
我们确定了 CICU 中的患者,这些患者有可用的超声心动图数据。LVSD 定义为左心室射血分数 < 40%,RVSD 定义为半定量测量中度或更大程度的收缩功能障碍,BVD 定义为两者都存在。多变量逻辑回归确定了心室功能障碍与调整后的住院死亡率之间的关系,作为 SCAI 分期的函数。
结果
研究人群包括 3,158 名患者,平均 ± SD 年龄为 68.2 ± 14.6 岁,其中 51.8% 患有急性冠状动脉综合征。LVSD 占 22.3%,RVSD 占 11.8%,BVD 占 16.4%。调整 SCAI 休克分期后,LVSD 或 RVSD 患者与无心室功能障碍患者的住院死亡率无差异(P > .05),但 BVD 与较高的住院死亡率独立相关(调整后的风险比, 1.815;95% CI,1.237-2.663;P = .0023)。在 SCAI 分期标准中增加心室功能障碍增加了对住院死亡率的区分(受试者工作特征曲线下面积,0.784 对 0.766;P < .001)。
解释
在入住 CICU 的患者中,只有 BVD 与较高的住院死亡率独立相关。在 SCAI 休克标准中增加超声心动图评估可能有助于改善临床风险分层。



























 京公网安备 11010802027423号
京公网安备 11010802027423号