Seminars in Thoracic and Cardiovascular Surgery ( IF 2.6 ) Pub Date : 2021-09-20 , DOI: 10.1053/j.semtcvs.2021.09.006 Priya Giridhara 1 , Amitabh Poonia 1 , Deepa S Kumar 1 , Anoop Ayyappan 2 , Kavassery M Krishnamoorthy 1 , Sivasankaran Sivasubramonian 1 , Ajitkumar Valaparambil 1
|
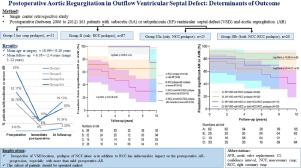
Aortic cusp prolapse is an acquired complication and usually precedes the development of aortic regurgitation (AR) in unoperated outflow ventricular septal defect (VSD). However, its impact on postoperative AR-progression is unknown. 161 patients with outflow-VSD and AR who underwent surgery between 2006 and 2012 were studied retrospectively. 31 patients without prolapse (group-I), 87 with only right coronary cusp (RCC) (group-II), 43 with noncoronary cusp (NCC) prolapse (group-III: 23 only NCC (IIIa), 20 both NCC-RCC (IIIb)) were followed postoperatively for a mean 6.05 ± 2.4 years (range 3–12 years). Moderate or severe-AR was present in 4.2%, 36.8%, 52.2% and 80% preoperatively; in 3.2%, 10.3%, 39.1% and 30% patients at follow-up in group-I, II, IIIa, and IIIb, respectively. Although freedom from significant-AR (moderate or severe AR) or aortic valve replacement (AVR) at 10 years was lesser in subaortic-VSD than subpulmonic-VSD (64.3 ± 7.5% vs 87.9 ± 3.6%; P = 0.02), the difference was not significant when compared within prolapse groups (80 ± 8% vs 88.7 ± 4.0%, P = 0.28 in group-II; 40.7 ± 11.8 vs 70 ± 14.5%, P = 0.48 in group-III). The significant-AR or AVR free survival in patients with trivial or mild preoperative-AR was not significantly different between prolapse groups (98.2 ± 1.8% vs 75 ± 21.7% in group-II and III respectively; P = 0.85). However, in those with moderate or severe preoperative-AR it was significantly lesser in group-III than II (30.1 ± 9.8% vs 65.6 ± 8.4%, respectively; P = 0.04). Group-III, compare to group-II, had 3.28 and 5.24-time risk of development of significant-AR or requirement of AVR, respectively. Prolapse of NCC alone or in addition to RCC prolapse has unfavourable impact on the postoperative outcomes, especially in subaortic-VSD after development of more than mild AR preoperatively.
中文翻译:

流出道室间隔缺损的术后主动脉瓣关闭不全:结果的决定因素
主动脉瓣脱垂是一种获得性并发症,通常在未经手术的流出道室间隔缺损 (VSD) 中发生主动脉瓣关闭不全 (AR) 之前。然而,它对术后 AR 进展的影响尚不清楚。回顾性研究了 2006 年至 2012 年间接受手术的 161 例流出道型 VSD 和 AR 患者。31 名无脱垂的患者(I 组),87 名仅有右冠状动脉瓣尖(RCC)的患者(II 组),43 名无冠状动脉瓣尖(NCC)脱垂的患者(III 组:23 名仅有 NCC(IIIa),20 名同时有 NCC-RCC (IIIb)) 术后平均随访 6.05 ± 2.4 年(范围 3-12 年)。术前中度或重度 AR 占 4.2%、36.8%、52.2% 和 80%;在 I、II、IIIa 和 IIIb 组的随访中,分别有 3.2%、10.3%、39.1% 和 30% 的患者。P = 0.02),在脱垂组内比较时差异不显着(80 ± 8% vs 88.7 ± 4.0%, P = 0.28 in group-II; 40.7 ± 11.8 vs 70 ± 14.5%, P = 0.48 in group-III )。轻度或轻度术前 AR 患者的显着 AR 或 AVR 无生存率在脱垂组之间没有显着差异(组 II 和 III 分别为 98.2 ± 1.8% 和 75 ± 21.7%;P = 0.85)。然而,在中度或重度术前 AR 的患者中,III 组明显低于 II 组(分别为 30.1 ± 9.8% 和 65.6 ± 8.4%;P = 0.04)。与第二组相比,第三组发生显着 AR 或需要 AVR 的风险分别为 3.28 和 5.24 倍。单独的 NCC 脱垂或除了 RCC 脱垂之外的脱垂对术后结果有不利影响,特别是在术前发生超过轻度 AR 后的主动脉下-VSD 中。











































 京公网安备 11010802027423号
京公网安备 11010802027423号