Bioactive Materials ( IF 18.0 ) Pub Date : 2021-09-15 , DOI: 10.1016/j.bioactmat.2021.09.011 Junjun Yang 1 , Xin Wang 1 , Yahan Fan 2 , Xiongbo Song 1 , Jiangyi Wu 3 , Zhenlan Fu 1 , Tao Li 1 , Yang Huang 1 , ZheXiong Tang 1 , Shuo Meng 4 , Na Liu 1, 5 , Jiajia Chen 6 , Pingju Liu 7 , Liu Yang 1 , Xiaoyuan Gong 1 , Cheng Chen 4
|
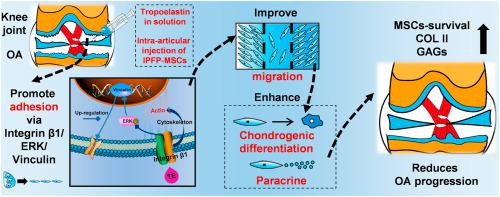
Intra-articular injection of mesenchymal stem cells (MSCs) is a promising strategy for osteoarthritis (OA) treatment. However, more and more studies reveal that the injected MSCs have poor adhesion, migration, and survival in the joint cavity. A recent study shows that tropoelastin (TE) regulates adhesion, proliferation and phenotypic maintenance of MSCs as a soluble additive, indicating that TE could promote MSCs-homing in regenerative medicine. In this study, we used TE as injection medium, and compared it with classic media in MSCs intra-articular injection such as normal saline (NS), hyaluronic acid (HA), and platelet-rich plasma (PRP). We found that TE could effectively improve adhesion, migration, chondrogenic differentiation of infrapatellar fat pad MSCs (IPFP-MSCs) and enhance matrix synthesis of osteoarthritic chondrocytes (OACs) in indirect-coculture system. Moreover, TE could significantly enhance IPFP-MSCs adhesion via activation of integrin β1, ERK1/2 and vinculin (VCL) in vitro. In addition, intra-articular injection of TE-IPFP MSCs suspension resulted in a short-term increase in survival rate of IPFP-MSCs and better histology scores of rat joint tissues. Inhibition of integrin β1 or ERK1/2 attenuated the protective effect of TE-IPFP MSCs suspension in vivo. In conclusion, TE promotes performance of IPFP-MSCs and protects knee cartilage from damage in OA through enhancement of cell adhesion and activation of integrin β1/ERK/VCL pathway. Our findings may provide new insights in MSCs intra-articular injection for OA treatment.
中文翻译:

原弹性蛋白改善关节内注射的髌下脂肪垫间充质干细胞的粘附和迁移,并减少骨关节炎的进展
关节内注射间充质干细胞 (MSCs) 是治疗骨关节炎 (OA) 的一种很有前景的策略。然而,越来越多的研究表明,注射的MSCs在关节腔内的粘附、迁移和存活能力较差。最近的一项研究表明,原弹性蛋白 (TE) 作为可溶性添加剂调节 MSCs 的粘附、增殖和表型维持,表明 TE 可以促进 MSCs 在再生医学中的归巢。在本研究中,我们使用 TE 作为注射介质,并将其与 MSCs 关节内注射中的经典介质进行比较,例如生理盐水 (NS)、透明质酸 (HA) 和富含血小板的血浆 (PRP)。我们发现 TE 可以有效提高附着力、迁移、在间接共培养系统中,髌下脂肪垫间充质干细胞 (IPFP-MSCs) 的软骨形成分化和增强骨关节炎软骨细胞 (OACs) 的基质合成。此外,TE可以通过激活整合素β1、ERK1/2和纽蛋白(VCL)显着增强IPFP-MSCs的粘附体外。此外,关节内注射 TE-IPFP MSCs 悬浮液导致 IPFP-MSCs 存活率的短期增加和更好的大鼠关节组织的组织学评分。抑制整合素 β1 或 ERK1/2 减弱了体内TE-IPFP MSCs 悬浮液的保护作用。总之,TE 通过增强细胞粘附和激活整合素 β1/ERK/VCL 通路来促进 IPFP-MSC 的性能并保护膝关节软骨免受 OA 损伤。我们的发现可能为 MSCs 关节内注射治疗 OA 提供新的见解。











































 京公网安备 11010802027423号
京公网安备 11010802027423号