The Journal of Thoracic and Cardiovascular Surgery ( IF 4.9 ) Pub Date : 2021-08-25 , DOI: 10.1016/j.jtcvs.2021.07.049 Shinichi Fukuhara 1 , Minhaj S Khaja 2 , David M Williams 3 , Xhorlina Marko 3 , Bo Yang 1 , Himanshu J Patel 1 , Karen M Kim 1
|
Objective
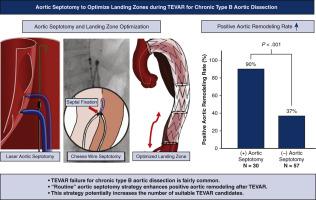
The role of thoracic endovascular aortic repair for chronic type B aortic dissection remains controversial. Clinical outcomes of thoracic endovascular aortic repair with recently implemented aortic septotomy strategy were compared with stand-alone thoracic endovascular aortic repair.
Methods
Between 2008 and 2020, 88 patients with chronic type B aortic dissection and degenerative aortic aneurysm underwent a thoracic endovascular aortic repair with or without adjunctive aortic septotomy, consisting of 36 (41%) with de novo chronic type B aortic dissection and 52 (59%) with residual chronic type B aortic dissection after type A aortic dissection repair.
Results
Aortic septotomy was performed in 31 patients (35%) to optimize the proximal (3/31;10%) and distal (31/31;100%) landing zones. The aortic septotomy techniques comprised laser aortic septotomy in 16 patients (52%) and cheese wire septotomy in 15 patients (48%) with a 97% overall technical success rate. The median time interval between aortic dissection occurrence and thoracic endovascular aortic repair was 1.2 years. During follow-up, there were 12 (21%) sudden deaths and 17 (30%) combined aorta-related and sudden deaths in the nonaortic septotomy group, whereas there were no deaths in the septotomy group (P < .001). Patients without aortic septotomy required aortic reinterventions more frequently than those with aortic septotomy (30% vs 7%; P = .014), and 77% of these procedures were related to residual retrograde false lumen flow. Positive aortic remodeling was confirmed in 90% and 37% in the aortic septotomy and nonseptotomy groups, respectively (P < .001).
Conclusions
Stand-alone thoracic endovascular aortic repair outcomes without adjunctive procedures for chronic type B aortic dissection remain unfavorable. In contrast, landing zone optimization using aortic septotomy resulted in a remarkably higher positive aortic remodeling rate. Routine aortic septotomy strategy may positively affect long-term chronic type B aortic dissection survival and expand thoracic endovascular aortic repair candidacy.
中文翻译:

主动脉隔切术优化慢性 B 型主动脉夹层胸主动脉腔内修复过程中的着陆区
客观的
胸腔主动脉腔内修复对慢性 B 型主动脉夹层的作用仍存在争议。将最近实施的主动脉隔切术策略的胸主动脉腔内修复术的临床结果与独立的胸主动脉腔内修复术进行了比较。
方法
2008 年至 2020 年间,88 名患有慢性 B 型主动脉夹层和退行性主动脉瘤的患者接受了胸主动脉腔内修复术,有或没有辅助主动脉中隔切开术,其中 36 名 (41%) 患有新发慢性 B 型主动脉夹层,52 名 (59%) ) A 型主动脉夹层修复术后残留慢性 B 型主动脉夹层。
结果
31 名患者 (35%) 进行了主动脉中隔切开术,以优化近端 (3/31;10%) 和远端 (31/31;100%) 着陆区。主动脉隔膜切开术包括 16 例患者 (52%) 的激光主动脉隔膜切开术和 15 例患者 (48%) 的粗纱线隔膜切开术,总体技术成功率为 97%。主动脉夹层发生与胸主动脉腔内修复术之间的中位时间间隔为 1.2 年。在随访期间,非主动脉隔切术组有 12 例 (21%) 猝死和 17 例 (30%) 合并主动脉相关和猝死,而切开术组没有死亡 (P < . 001 )。未行主动脉中隔切开术的患者比行主动脉中隔切开术的患者需要更频繁地进行主动脉再介入治疗(30% 对 7%;P = .014),并且这些手术中有 77% 与残余逆行假腔流有关。在主动脉中隔切开术和非中隔切开术组中,分别有 90% 和 37% 的主动脉重塑阳性 ( P < . 001)。
结论
慢性 B 型主动脉夹层没有辅助手术的独立胸主动脉血管内修复结果仍然不利。相比之下,使用主动脉隔膜切开术优化着陆区可显着提高正主动脉重塑率。常规主动脉中隔切开策略可能对慢性 B 型主动脉夹层的长期存活率产生积极影响,并扩大胸主动脉腔内修复术的候选范围。











































 京公网安备 11010802027423号
京公网安备 11010802027423号