Journal of Hepatology ( IF 26.8 ) Pub Date : 2021-08-24 , DOI: 10.1016/j.jhep.2021.08.007 Julien Vionnet 1 , Rosa Miquel 2 , Juan G Abraldes 3 , Jurate Wall 4 , Elisavet Kodela 4 , Juan-Jose Lozano 5 , Pablo Ruiz 6 , Miguel Navasa 6 , Aileen Marshall 7 , Frederik Nevens 8 , Will Gelson 9 , Joanna Leithead 9 , Steven Masson 10 , Elmar Jaeckel 11 , Richard Taubert 11 , Phaedra Tachtatzis 12 , Dennis Eurich 13 , Kenneth J Simpson 14 , Eliano Bonaccorsi-Riani 15 , Sandy Feng 16 , John Bucuvalas 17 , James Ferguson 18 , Alberto Quaglia 7 , Julia Sidorova 19 , Maria Elstad 20 , Abdel Douiri 20 , Alberto Sánchez-Fueyo 4
|
Background & Aims
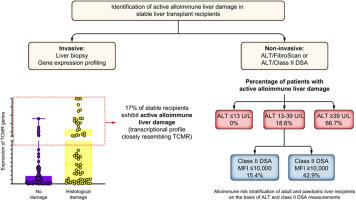
Management of long-term immunosuppression following liver transplantation (LT) remains empirical. Surveillance liver biopsies in combination with transcriptional profiling could overcome this challenge by identifying recipients with active alloimmune-mediated liver damage despite normal liver tests, but this approach lacks applicability. Our aim was to investigate the utility of non-invasive tools for the stratification of stable long-term survivors of LT, according to their immunological risk and need for immunosuppression.
Methods
We conducted a cross-sectional multicentre study of 190 adult LT recipients assessed to determine their eligibility to participate in an immunosuppression withdrawal trial. Patients had stable liver allograft function and had been transplanted for non-autoimmune non-replicative viral liver disease >3 years before inclusion. We performed histological, immunogenetic and serological studies and measured the intrahepatic transcript levels of an 11-gene classifier highly specific for T cell-mediated rejection (TCMR).
Results
In this cohort, 35.8% of patients harboured clinically silent fibro-inflammatory liver lesions (13.7% had mild damage and 22.1% had moderate-to-severe damage). The severity of liver allograft damage was positively associated with TCMR-related transcripts, class II donor-specific antibodies (DSAs), ALT, AST, and liver stiffness measurement (LSM), and negatively correlated with serum creatinine and tacrolimus trough levels. Liver biopsies were stratified according to their TCMR transcript levels using a cut-off derived from biopsies with clinically significant TCMR. Two multivariable prediction models, integrating ALT+LSM or ALT+class II DSAs, had a high discriminative capacity for classifying patients with or without alloimmune damage. The latter model performed well in an independent cohort of 156 liver biopsies obtained from paediatric liver recipients with similar inclusion/exclusion criteria.
Conclusion
ALT, class II DSAs and LSM are valuable tools to non-invasively identify stable LT recipients without significant underlying alloimmunity who could benefit from minimisation of immunosuppression.
Lay summary
A large proportion of liver transplant patients with normal liver tests have inflammatory liver lesions, which in 17% of cases are molecularly indistinguishable from those seen at the time of rejection. ALT, class II donor-specific antibodies and liver stiffness are useful in identifying patients with this form of subclinical rejection. We propose these markers as a useful tool to help clinicians determine if the immunosuppression administered is adequate.
中文翻译:

长期肝移植受者的无创同种免疫风险分层
背景与目标
肝移植 (LT) 后长期免疫抑制的管理仍然是经验性的。尽管肝脏测试正常,但监测肝活检结合转录分析可以通过识别具有活性同种免疫介导的肝损伤的受体来克服这一挑战,但这种方法缺乏适用性。我们的目的是根据免疫风险和免疫抑制需求,研究非侵入性工具对 LT 稳定长期幸存者进行分层的效用。
方法
我们对 190 名成年 LT 接受者进行了一项横断面多中心研究,评估以确定他们是否有资格参加免疫抑制戒断试验。患者具有稳定的肝脏同种异体移植功能,并且在纳入前已因非自身免疫性非复制性病毒性肝病>3 年进行移植。我们进行了组织学、免疫遗传学和血清学研究,并测量了对 T 细胞介导的排斥 (TCMR) 具有高度特异性的 11 基因分类器的肝内转录水平。
结果
在该队列中,35.8% 的患者存在临床上无症状的纤维炎症性肝损伤(13.7% 有轻度损伤,22.1% 有中度至重度损伤)。肝移植损伤的严重程度与 TCMR 相关转录本、II 类供体特异性抗体 (DSA)、ALT、AST 和肝硬度测量 (LSM) 呈正相关,与血清肌酐和他克莫司谷水平呈负相关。使用从具有临床意义的 TCMR 的活检获得的截止值,根据其 TCMR 转录水平对肝活检进行分层。两个多变量预测模型,整合了 ALT+LSM 或 ALT+II 类 DSA,对有或没有同种免疫损伤的患者进行分类具有很高的判别能力。
结论
ALT、II 类 DSA 和 LSM 是无创识别稳定的 LT 受者的宝贵工具,这些受者没有显着的潜在同种免疫,可以从免疫抑制的最小化中受益。
总结
大部分肝脏检查正常的肝移植患者有炎症性肝脏病变,其中 17% 的病例在分子上与排斥时所见的那些无法区分。ALT、II 类供体特异性抗体和肝脏硬度可用于识别具有这种亚临床排斥反应的患者。我们建议将这些标志物作为一种有用的工具来帮助临床医生确定所给予的免疫抑制是否足够。











































 京公网安备 11010802027423号
京公网安备 11010802027423号