JACC: Heart Failure ( IF 10.3 ) Pub Date : 2021-08-23 , DOI: 10.1016/j.jchf.2021.06.017 John J V McMurray 1 , David C Wheeler 2 , Bergur V Stefánsson 3 , Niels Jongs 4 , Douwe Postmus 5 , Ricardo Correa-Rotter 6 , Glenn M Chertow 7 , Fan Fan Hou 8 , Peter Rossing 9 , C David Sjöström 3 , Scott D Solomon 10 , Robert D Toto 11 , Anna Maria Langkilde 3 , Hiddo J L Heerspink 12 ,
|
Objectives
The purpose of this paper was to investigate the effects of dapagliflozin in chronic kidney disease (CKD) patients, with and without heart failure (HF).
Background
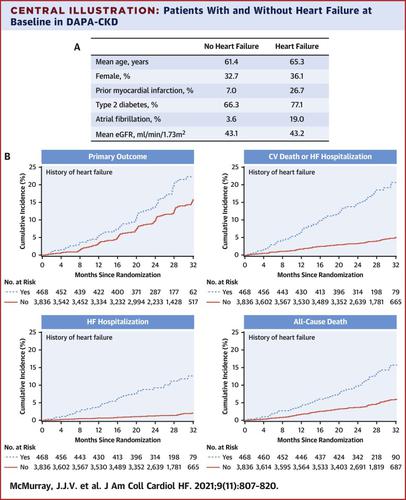
Patients with CKD, with and without type 2 diabetes, were enrolled in the DAPA-CKD (Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease) trial. Some patients had HF at baseline.
Methods
A total of 4,304 participants were randomized to dapagliflozin 10 mg daily or placebo. The primary composite endpoint was ≥50% decline in estimated glomerular filtration rate, end-stage kidney disease, or kidney/cardiovascular death. Secondary endpoints were a kidney composite (primary endpoint minus cardiovascular death), the composite of cardiovascular death/HF hospitalization, and all-cause death. Analysis of outcomes according to HF history was prespecified.
Results
HF patients (n = 468; 11%) were older and had more coronary disease, atrial fibrillation, and type 2 diabetes. Mean estimated glomerular filtration rate was similar in patients with and without HF. Rates of HF hospitalization/cardiovascular death and death from any cause were higher in HF patients, but the secondary kidney failure outcome occurred at the same rate in people with and without HF. Dapagliflozin reduced the risk of the primary outcome equally in patients with HF (HR: 0.58 [95% CI: 0.37-0.91]) and without HF (HR: 0.62 [95% CI: 0.51-0.75]) (P interaction = 0.59). The proportional risk-reductions were similar in patients with and without HF for the cardiovascular death/HF hospitalization composite (HR: 0.68 [95% CI: 0.44-1.05] vs HR: 0.70 [95% CI: 0.51-0.97], respectively; P interaction = 0.90), and all-cause death (HR: 0.56 [95% CI: 0.34-0.93] vs HR: 0.73 [95% CI: 0.54-0.97], respectively; P interaction = 0.39), although absolute risk reductions were larger in HF patients. Adverse event rates were low and did not differ among patients with or without HF.
Conclusions
Dapagliflozin reduced the risk of kidney failure and cardiovascular death/HF hospitalization and prolonged survival in CKD patients with or without type 2 diabetes, independently of history of HF. (A Study to Evaluate the Effect of Dapagliflozin on Renal Outcomes and Cardiovascular Mortality in Patients With Chronic Kidney Disease [DAPA-CKD]; NCT03036150)
中文翻译:

达格列净对肾病、心力衰竭和心力衰竭患者的影响
目标
本文的目的是研究达格列净对慢性肾脏病 (CKD) 患者的影响,无论是否伴有心力衰竭 (HF)。
背景
患有和不患有 2 型糖尿病的 CKD 患者参加了 DAPA-CKD(达格列净和预防慢性肾病不良结局)试验。一些患者在基线时有 HF。
方法
共有 4,304 名参与者被随机分配至 dapagliflozin 10 mg 每日或安慰剂组。主要复合终点是估计肾小球滤过率下降≥50%、终末期肾病或肾/心血管死亡。次要终点是肾脏复合终点(主要终点减去心血管死亡)、心血管死亡/心衰住院的复合终点和全因死亡。预先指定了根据 HF 病史对结果的分析。
结果
HF 患者(n = 468;11%)年龄较大,冠心病、心房颤动和 2 型糖尿病的发生率更高。HF 和非 HF 患者的平均估计肾小球滤过率相似。HF 患者的 HF 住院/心血管死亡和全因死亡率较高,但继发性肾衰竭结果在患有和不患有 HF 的人群中发生率相同。达格列净降低 HF 患者(HR:0.58 [95% CI:0.37-0.91])和非 HF(HR:0.62 [95% CI:0.51-0.75])患者主要结局的风险相同(P交互作用 = 0.59) . 对于心血管死亡/心衰住院复合患者,心衰患者和非心衰患者的风险降低比例相似(分别为 HR:0.68 [95% CI:0.44-1.05] vs HR:0.70 [95% CI:0.51-0.97];磷交互作用 = 0.90)和全因死亡(HR:0.56 [95% CI:0.34-0.93] 与 HR:0.73 [95% CI:0.54-0.97],分别;P交互作用 = 0.39),尽管绝对风险降低HF 患者更大。不良事件发生率很低,并且在有或没有 HF 的患者中没有差异。
结论
达格列净降低了伴或不伴 2 型糖尿病的 CKD 患者的肾衰竭和心血管死亡/心衰住院风险,并延长了生存期,与心衰史无关。(一项评估达格列净对慢性肾病患者肾脏结局和心血管死亡率影响的研究 [DAPA-CKD];NCT03036150)









































 京公网安备 11010802027423号
京公网安备 11010802027423号