Atherosclerosis ( IF 4.9 ) Pub Date : 2021-08-14 , DOI: 10.1016/j.atherosclerosis.2021.08.016 Caitlin W Hicks 1 , Ada Al-Qunaibet 2 , Ning Ding 3 , Lucia Kwak 3 , Aaron R Folsom 4 , Hirofumi Tanaka 5 , Thomas Mosley 6 , Lynne E Wagenknecht 7 , Weihong Tang 4 , Gerardo Heiss 8 , Kunihiro Matsushita 3
|
Background and aims
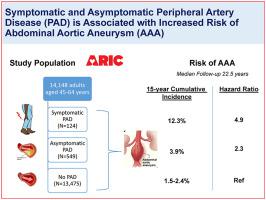
Symptomatic peripheral artery disease (PAD) is a risk factor for abdominal aortic aneurysm (AAA). However, data on the association of asymptomatic PAD with AAA are limited. We explored the association of symptomatic and asymptomatic PAD with AAA.
Methods
We primarily assessed a prospective association of symptomatic (based on clinical history) and asymptomatic (ankle-brachial index ≤0.9) PAD at baseline (1987–89 [ages 45–64 years]) with incident AAA in a biracial community-based cohort, the Atherosclerosis Risk in Communities Study. We secondarily investigated a cross-sectional association of PAD with ultrasound-based AAA (diameter≥3.0 cm) (2011–13 [ages 67–91 years]).
Results
Of 14,148 participants (55.1% female, 25.5% black, 0.9% with symptomatic PAD) in our prospective analysis (median follow-up 22.5 years), 530 (3.7%) developed incident AAA. Symptomatic PAD had a higher hazard ratio (HR) of incident AAA [4.91 (95%CI 2.88–8.37)], as did asymptomatic PAD with ABI≤0.9 [2.33 (1.55–3.51)], compared to the reference ABI>1.1–1.2 in demographically-adjusted models. Crude 15-year cumulative incidence of AAA in these three groups were 12.3%, 3.9%, and 1.5%, respectively. The associations remained significant after accounting for other potential confounders [corresponding HR 2.96 (95%CI 1.73–5.07) and 1.52 (95%CI 1.00–2.30), respectively]. The cross-sectional analysis demonstrated similar patterns with ultrasound-based AAA [odds ratio 2.46 (95%CI 1.26–4.81) for symptomatic PAD and 3.98 (1.96–8.08) for asymptomatic PAD in a demographically-adjusted model].
Conclusions
Our prospective and cross-sectional data show elevated risk of AAA in both symptomatic and asymptomatic PAD. Our data support the current recommendation of AAA screening in symptomatic PAD patients and suggest the potential extension to asymptomatic PAD patients as well.
中文翻译:

有症状和无症状外周动脉疾病以及腹主动脉瘤的风险:社区动脉粥样硬化风险 (ARIC) 研究
背景和目标
症状性外周动脉疾病(PAD)是腹主动脉瘤(AAA)的危险因素。然而,有关无症状 PAD 与 AAA 关联的数据有限。我们探讨了有症状和无症状 PAD 与 AAA 的关联。
方法
我们主要在一个基于混血社区的队列中评估了基线(1987-89 [年龄 45-64 岁])有症状(基于临床病史)和无症状(踝臂指数≤0.9)PAD 与 AAA 事件的前瞻性关联,社区动脉粥样硬化风险研究。我们其次研究了 PAD 与基于超声的 AAA(直径≥3.0 cm)的横断面关联(2011-13 [年龄 67-91 岁])。
结果
在我们的前瞻性分析(中位随访时间 22.5 年)中,14,148 名参与者(55.1% 为女性,25.5% 为黑人,0.9% 患有有症状的 PAD)中,530 名(3.7%)发生了 AAA。与参考 ABI>1 相比,有症状的 PAD 发生 AAA 的风险比 (HR) 较高 [4.91 (95%CI 2.88–8.37)],ABI≤0.9 的无症状 PAD 也是如此 [2.33 (1.55–3.51)]。人口调整模型中的 1–1.2。这三组 AAA 的 15 年粗累积发生率分别为 12.3%、3.9% 和 1.5%。考虑到其他潜在的混杂因素后,这种关联仍然显着[相应的 HR 分别为 2.96 (95% CI 1.73–5.07) 和 1.52 (95% CI 1.00–2.30)]。横断面分析表明,基于超声的 AAA 具有相似的模式 [在人口统计调整模型中,有症状 PAD 的比值比为 2.46 (95% CI 1.26–4.81),无症状 PAD 的比值比为 3.98 (1.96–8.08)]。
结论
我们的前瞻性和横断面数据显示,有症状和无症状 PAD 的 AAA 风险均升高。我们的数据支持目前对有症状的 PAD 患者进行 AAA 筛查的建议,并表明也可能扩展到无症状的 PAD 患者。











































 京公网安备 11010802027423号
京公网安备 11010802027423号