Atherosclerosis ( IF 4.9 ) Pub Date : 2021-08-05 , DOI: 10.1016/j.atherosclerosis.2021.08.007 Martino Pepe 1 , Gianluigi Napoli 1 , Eugenio Carulli 1 , Marco Moscarelli 2 , Cinzia Forleo 1 , Palma Luisa Nestola 1 , Giuseppe Biondi-Zoccai 3 , Arturo Giordano 4 , Stefano Favale 1
|
Background and aims
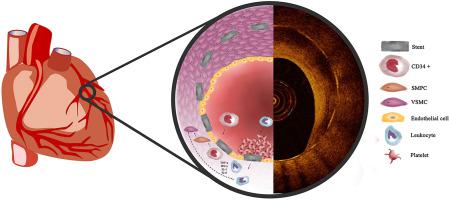
Despite the relation between autoimmune diseases and increased atherosclerotic risk is established, the influence of autoimmune disorders on in-stent restenosis (ISR) after percutaneous coronary intervention (PCI) is only partly known. ISR is an aberrant reparative process mainly characterized by an increased number of vascular smooth muscle cells and excessive deposition of extracellular proteoglycans and type III collagen. Chronic inflammation, always present in autoimmune diseases, modulates the endothelial response to PCI. Aim of this review is to resume the current evidence on the association between ISR and autoimmune diseases, focusing on pathogenic mechanisms and therapeutic targets.
Methods
We conducted a comprehensive review of the literature on the relationship between ISR and insulin-dependent diabetes mellitus (IDDM), rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), antiphospholipid-antibodies syndrome (APS), inflammatory bowel diseases (IBD), and Hashimoto's thyroiditis (HT).
Results
Patients affected with IDDM, RA, SLE, APS, IBD and HT proved to face higher rates of ISR compared to the general population. The endothelial dysfunction seems the principal common pathogenic pathway for ISR and is attributed to both the immune system disorder and the systemic inflammation. Some evidence suggested that methotrexate and anti-tumor necrosis factor treatments can be effective in reducing ISR, while antibodies against vascular cell adhesion molecule-1 and intercellular adhesion molecule-1 showed to reduce neointimal hyperplasia in animal models.
Conclusions
Autoimmune diseases are a risk factor for ISR. The study of the potential cardiovascular benefits of the current therapies, mainly anti-inflammatory drugs, and the pursuit of innovative treatments appear of paramount interest.
中文翻译:

接受经皮冠状动脉介入治疗患者的自身免疫性疾病:支架内再狭窄的危险因素?
背景和目标
尽管已确定自身免疫性疾病与动脉粥样硬化风险增加之间的关系,但仅部分了解自身免疫性疾病对经皮冠状动脉介入治疗 (PCI) 后支架内再狭窄 (ISR) 的影响。ISR 是一种异常的修复过程,主要特征是血管平滑肌细胞数量增加以及细胞外蛋白聚糖和 III 型胶原蛋白的过度沉积。自身免疫性疾病中始终存在的慢性炎症调节内皮对 PCI 的反应。本综述的目的是恢复关于 ISR 与自身免疫性疾病之间关联的当前证据,重点是发病机制和治疗靶点。
方法
我们对 ISR 与胰岛素依赖型糖尿病 (IDDM)、类风湿性关节炎 (RA)、系统性红斑狼疮 (SLE)、抗磷脂抗体综合征 (APS)、炎症性肠病 (IBD) 之间关系的文献进行了全面回顾和桥本氏甲状腺炎 (HT)。
结果
与一般人群相比,受 IDDM、RA、SLE、APS、IBD 和 HT 影响的患者面临更高的 ISR 发生率。内皮功能障碍似乎是 ISR 的主要常见致病途径,可归因于免疫系统疾病和全身炎症。一些证据表明,甲氨蝶呤和抗肿瘤坏死因子治疗可有效降低 ISR,而抗血管细胞粘附分子 1 和细胞间粘附分子 1 的抗体在动物模型中显示可减少新生内膜增生。
结论
自身免疫性疾病是 ISR 的危险因素。对当前疗法(主要是抗炎药)的潜在心血管益处的研究以及对创新疗法的追求显得尤为重要。











































 京公网安备 11010802027423号
京公网安备 11010802027423号