当前位置:
X-MOL 学术
›
Lett. Appl. Microbiol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Analysis of antibiotic resistance and virulence patterns in Klebsiella pneumoniae isolated from human urinary tract infections in India
Letters in Applied Microbiology ( IF 2.0 ) Pub Date : 2021-07-31 , DOI: 10.1111/lam.13544 S Bobbadi 1 , B K Chinnam 2 , P N Reddy 1 , S Kandhan 3
Letters in Applied Microbiology ( IF 2.0 ) Pub Date : 2021-07-31 , DOI: 10.1111/lam.13544 S Bobbadi 1 , B K Chinnam 2 , P N Reddy 1 , S Kandhan 3
Affiliation
|
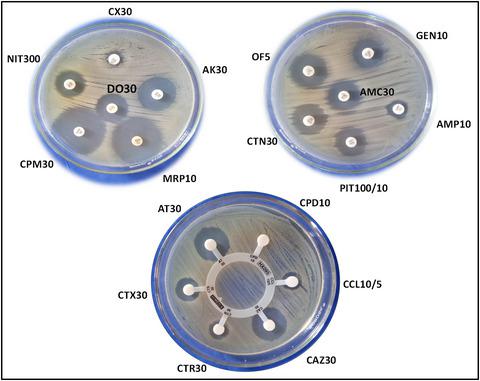
In this study, 504 urine samples collected from patients suffering from urinary tract infection (UTIs) were screened for the presence of Klebsiella pneumoniae. The overall occurrence of Klebsiella spp. and K. pneumoniae was found to be 23·2% (117/504) and 16·8% (85/504) respectively. Antibiotic susceptibility testing of 85 K. pneumoniae isolates was carried out by disc diffusion which revealed alarming levels of antibiotic resistance (ABR). Antimicrobial resistance was prominently observed against cefpodoxime (76·47%) followed by ampicillin (70·59%), ceftriaxone (52·94%), cefoxitin (50·59%), amoxyclav (48·24%), ofloxacin (45·88%), cefotaxime (44·71%), cefepime (43·53%) and doxycycline hydrochloride (40%). A small percentage of strains also exhibited resistance to other antimicrobials in the range of 7–35%. Around 77·6% of the isolates were found to be resistant to three or more antibiotic classes and 66·7% of the isolates had multiple antibiotic resistance index values >0·2. Screening of virulence genes in 85 K. pneumoniae isolates revealed that uge gene was the most predominant (11/85, 12·9%), followed by rmpA (9/85, 10·5%), kfu (4/85, 4·7%) and aerobactin genes (2/85, 2·35%). Further, the overall percentage of biofilm producers were found to be 17·65% (15/85). This study warrants hospitals and health care centres to reduce misuse of antibiotics and manage UTI with appropriate treatment after performing antibiotic susceptibility testing.
中文翻译:

印度人尿路感染中分离出的肺炎克雷伯菌的抗生素耐药性和毒力模式分析
在这项研究中,对从患有尿路感染 (UTI) 的患者收集的 504 份尿液样本进行了筛查,以确定是否存在肺炎克雷伯菌。克雷伯氏菌属的总体发生率。和肺炎克雷伯菌分别为 23·2% (117/504) 和 16·8% (85/504)。85 K的抗生素药敏试验。肺炎链球菌分离株是通过圆盘扩散进行的,这揭示了令人震惊的抗生素耐药性 (ABR) 水平。对头孢泊肟(76·47%)的抗菌素耐药性显着观察到,其次是氨苄青霉素(70·59%)、头孢曲松(52·94%)、头孢西丁(50·59%)、阿莫西林(48·24%)、氧氟沙星(45 ·88%)、头孢噻肟(44·71%)、头孢吡肟(43·53%)、盐酸多西环素(40%)。一小部分菌株还表现出对其他抗菌剂的耐药性,范围为 7-35%。约77·6%的分离株对三种或更多类抗生素耐药,66·7%的分离株多重耐药指数>0·2。在 85 K中筛选毒力基因。肺炎链球菌分离物显示uge基因占主导地位(11/85, 12·9%),其次是rmpA(9/85, 10·5%)、kfu(4/85, 4·7%)和 aerobactin 基因(2/85, 2 ·35%)。此外,发现生物膜生产者的总体百分比为 17·65% (15/85)。这项研究保证医院和医疗保健中心在进行抗生素敏感性测试后减少抗生素的滥用并通过适当的治疗来管理尿路感染。
更新日期:2021-07-31
中文翻译:

印度人尿路感染中分离出的肺炎克雷伯菌的抗生素耐药性和毒力模式分析
在这项研究中,对从患有尿路感染 (UTI) 的患者收集的 504 份尿液样本进行了筛查,以确定是否存在肺炎克雷伯菌。克雷伯氏菌属的总体发生率。和肺炎克雷伯菌分别为 23·2% (117/504) 和 16·8% (85/504)。85 K的抗生素药敏试验。肺炎链球菌分离株是通过圆盘扩散进行的,这揭示了令人震惊的抗生素耐药性 (ABR) 水平。对头孢泊肟(76·47%)的抗菌素耐药性显着观察到,其次是氨苄青霉素(70·59%)、头孢曲松(52·94%)、头孢西丁(50·59%)、阿莫西林(48·24%)、氧氟沙星(45 ·88%)、头孢噻肟(44·71%)、头孢吡肟(43·53%)、盐酸多西环素(40%)。一小部分菌株还表现出对其他抗菌剂的耐药性,范围为 7-35%。约77·6%的分离株对三种或更多类抗生素耐药,66·7%的分离株多重耐药指数>0·2。在 85 K中筛选毒力基因。肺炎链球菌分离物显示uge基因占主导地位(11/85, 12·9%),其次是rmpA(9/85, 10·5%)、kfu(4/85, 4·7%)和 aerobactin 基因(2/85, 2 ·35%)。此外,发现生物膜生产者的总体百分比为 17·65% (15/85)。这项研究保证医院和医疗保健中心在进行抗生素敏感性测试后减少抗生素的滥用并通过适当的治疗来管理尿路感染。









































 京公网安备 11010802027423号
京公网安备 11010802027423号