Journal of Hepatology ( IF 26.8 ) Pub Date : 2021-07-30 , DOI: 10.1016/j.jhep.2021.07.020 Fanny Turon 1 , Ellen G Driever 2 , Anna Baiges 1 , Eira Cerda 3 , Ángeles García-Criado 4 , Rosa Gilabert 4 , Concepció Bru 4 , Annalisa Berzigotti 5 , Isabel Nuñez 4 , Lara Orts 1 , Juan Carlos Reverter 6 , Marta Magaz 1 , Genis Camprecios 1 , Pol Olivas 3 , Fabian Betancourt-Sanchez 3 , Valeria Perez-Campuzano 3 , Annabel Blasi 7 , Susana Seijo 3 , Enric Reverter 1 , Jaume Bosch 8 , Roger Borràs 9 , Virginia Hernandez-Gea 1 , Ton Lisman 2 , Juan Carlos Garcia-Pagan 1
|
Background & Aims
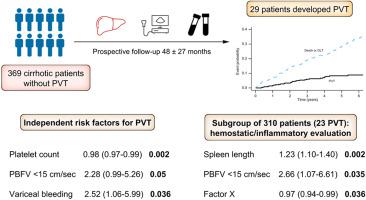
Portal vein thrombosis (PVT) is a relatively frequent event in patients with cirrhosis. While different risk factors for PVT have been reported, such as decreased portal blood flow velocity (PBFV) and parameters related with severity of portal hypertension, these are based on retrospective studies assessing only a discrete number of parameters. The aim of the current study was to evaluate the incidence and risks factors for non-tumoral PVT development in a large prospective cohort of patients with cirrhosis.
Methods
We performed an exhaustive evaluation of clinical, biochemical, inflammatory and acquired/hereditary hemostatic profiles in 369 patients with cirrhosis without PVT who were prospectively followed-up. Doppler ultrasound was performed at baseline and every 6 months or whenever clinically indicated. PVT development was always confirmed by computed tomography.
Results
Twenty-nine patients developed non-tumoral PVT, with an incidence of 1.6%, 6% and 8.4% at 1, 3 and 5 years, respectively. Low platelet count, PBFV <15 cm/sec and history of variceal bleeding were factors independently associated with a high PVT risk. No relationship between PVT development and any other clinical biochemical, inflammatory and acquired or hereditary hemostatic parameter was found.
Conclusions
In patients with cirrhosis, the factors predictive of PVT development were mainly those related to the severity of portal hypertension. Our results do not support the role of hemostatic alterations (inherited or acquired) and inflammatory markers in the prediction of PVT in patients with cirrhosis.
Lay summary
Patients with cirrhosis and more severe portal hypertension are at higher risk of non-tumoral portal vein thrombosis development. Acquired or inherited hemostatic disorders, as well as inflammatory status, do not seem to predict the development of portal vein thrombosis in patients with cirrhosis.
中文翻译:

预测肝硬化门静脉血栓形成:临床、超声和止血因素的前瞻性研究
背景与目标
门静脉血栓形成 (PVT) 是肝硬化患者相对常见的事件。虽然已经报道了 PVT 的不同危险因素,例如门静脉血流速度 (PBFV) 降低和与门静脉高压严重程度相关的参数,但这些都是基于仅评估离散数量参数的回顾性研究。本研究的目的是评估大型前瞻性肝硬化患者队列中非肿瘤性 PVT 发展的发生率和风险因素。
方法
我们对前瞻性随访的 369 名无 PVT 的肝硬化患者的临床、生化、炎症和获得性/遗传性止血特征进行了详尽的评估。在基线和每 6 个月或有临床指征时进行多普勒超声检查。PVT 的发展总是通过计算机断层扫描得到证实。
结果
29 名患者发生非肿瘤性 PVT,1、3 和 5 年的发病率分别为 1.6%、6% 和 8.4%。血小板计数低、PBFV <15 cm/sec 和静脉曲张出血史是与高 PVT 风险独立相关的因素。未发现 PVT 发展与任何其他临床生化、炎症和获得性或遗传性止血参数之间的关系。
结论
在肝硬化患者中,预测 PVT 发展的因素主要是与门静脉高压症严重程度相关的因素。我们的结果不支持止血改变(遗传性或获得性)和炎症标志物在预测肝硬化患者 PVT 中的作用。
总结
肝硬化和更严重的门静脉高压症患者发生非肿瘤性门静脉血栓形成的风险更高。获得性或遗传性止血障碍以及炎症状态似乎不能预测肝硬化患者门静脉血栓形成的发展。











































 京公网安备 11010802027423号
京公网安备 11010802027423号