Current HIV Research ( IF 0.8 ) Pub Date : 2021-08-31 , DOI: 10.2174/1570162x19666210726102027 Moses New-Aaron 1 , Happiness Kingi 2 , Jane L Meza 3 , Martha H Goedert 2 , Stephen M Kibusi 4 , Mkhoi L Mkhoi 5 , Caroline Damian Mayengo 6 , James Charles 6 , Siraji Shabani 6 , Temitope O New-Aaron 7 , Samwel Sumba 8 , Anlan Cheney 9
|
Background: The intention of antiretroviral therapy (ART) and regular clinic visits are to engender safe sex attitudes among HIV-infected individuals. However, this may not be the case due to the perceived therapeutic benefits of ART and may result in exposure to drug-resistant HIV strains.
Objectives: We aimed to determine the prevalence and predict the factors associated with risky sexual behaviors among ART users in a resource-limited environment.
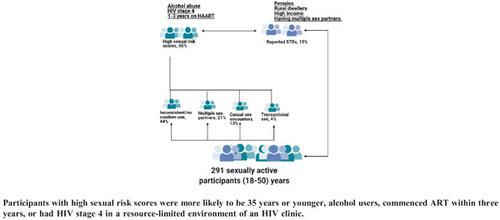
Methods: Two hundred and ninety-one sexually active ART-users aged 18-50 years and seeking care at the HIV clinic in Dodoma, Tanzania, participated in this study. The outcome variables modeled in a logistic regression were condom use, multiple sex partners, casual sex partners, and payment for sex. The predictors included in the models were the patients' socio-demographic characteristics. In addition, a new variable, sexual risk scores, was generated by culminating all the outcome variables. Finally, a multiple Poisson regression with the socio-demographic variables of the participants was used to model the sexual risk scores.
Results: Patients reported inconsistent/no condom use (44%), payment for sex (4%), casual sex encounters (13%), multiple sex partners (21%), and STD symptoms (15%). While having a casual sexual partner was significantly associated with age group in a Pearson Chi-square (p=0.0147), participants ≤35 years old were less likely to have single-sex partners than older participants (AOR: 0.188, 95 C.I: 0.042-0.849). Meanwhile, the likelihood of condom use was higher among participants with no HIV-infected family members (AOR= 2.409, 95% C.I:1.236,4.697) and among participants who had single-sex partners (AOR= 2.721, 95% C.I.: 1.115,6.640); these participants were less likely to report STD symptoms (AOR=0.265, 95% C.I.: 0.081-0.865). Adjusted analysis showed that estimated mean sexual risk scores significantly increased (mean, λ=1.61, 95% C.I:1.0817-2.4063) for recent ART recipients (within 1-3 years vs. ≥8 years). However, sexual risk scores of participants with HIV stage 3 were 38.8% lower than participants at stage 4 (95% C.I.: 0.3910-0.9558), and non-alcohol drinkers had an adjusted mean sexual risk score of 29% lower than participants who were alcohol drinkers (95% C.I.: 0.5102-0.9879).
Conclusion: Researchers should prioritize patients at HIV CTC for education concerning safe sexual practices for those characterized by alcohol consumption, younger age (less than 35 years old), HIV stage 4, or commencement of ART within three years.
中文翻译:

ART 持续时间、酒精使用和 HIV 阶段可能预测资源有限环境中的危险性行为:一项横断面研究
背景:抗逆转录病毒治疗 (ART) 和定期门诊就诊的目的是在 HIV 感染者中产生安全的性行为态度。然而,由于 ART 的治疗益处,情况可能并非如此,并且可能导致接触耐药性 HIV 毒株。
目的:我们旨在确定资源有限环境中 ART 用户中危险性行为的患病率并预测相关因素。
方法:291 名年龄在 18-50 岁的性活跃 ART 使用者并在坦桑尼亚多多马的 HIV 诊所寻求护理,参与了这项研究。在逻辑回归中建模的结果变量是安全套使用、多个性伴侣、临时性伴侣和性支付。模型中包含的预测因子是患者的社会人口学特征。此外,通过汇总所有结果变量,生成了一个新变量,即性风险评分。最后,使用参与者的社会人口变量进行多元泊松回归来模拟性风险评分。
结果:患者报告不一致/未使用安全套 (44%)、性支付 (4%)、偶然性接触 (13%)、多个性伴侣 (21%) 和 STD 症状 (15%)。虽然在 Pearson 卡方检验中,拥有随意性伴侣与年龄组显着相关(p=0.0147),但与年长的参与者相比,≤35 岁的参与者拥有单一性伴侣的可能性更低(AOR:0.188, 95 CI:0.042 -0.849)。同时,没有感染 HIV 的家庭成员(AOR= 2.409, 95% CI: 1.236,4.697)和有单性伴侣的参与者(AOR= 2.721, 95% CI: 1.115)使用安全套的可能性更高,6.640); 这些参与者不太可能报告 STD 症状 (AOR=0.265, 95% CI: 0.081-0.865)。调整后的分析表明,估计的平均性风险评分显着增加(平均值,λ=1.61,95% CI:1.0817-2。4063) 用于最近的 ART 接受者(1-3 年内 vs. ≥8 年)。然而,HIV 3 期参与者的性风险评分比第 4 期参与者低 38.8%(95% CI:0.3910-0.9558),非酒精饮酒者的调整后平均性风险评分比 HIV 4 期参与者低 29%。饮酒者(95% CI:0.5102-0.9879)。
结论:研究人员应优先考虑 HIV CTC 的患者,对以饮酒、年龄较小(小于 35 岁)、HIV 4 期或三年内开始 ART 为特征的患者进行安全性行为教育。











































 京公网安备 11010802027423号
京公网安备 11010802027423号