Kidney International ( IF 14.8 ) Pub Date : 2021-07-18 , DOI: 10.1016/j.kint.2021.07.005 Maxime Espi 1 , Xavier Charmetant 2 , Thomas Barba 3 , Laetitia Koppe 4 , Caroline Pelletier 5 , Emilie Kalbacher 5 , Elodie Chalencon 6 , Virginie Mathias 7 , Anne Ovize 8 , Emmanuelle Cart-Tanneur 8 , Christine Bouz 8 , Laurence Pellegrina 8 , Emmanuel Morelon 9 , Denis Fouque 4 , Laurent Juillard 10 , Olivier Thaunat 11
|
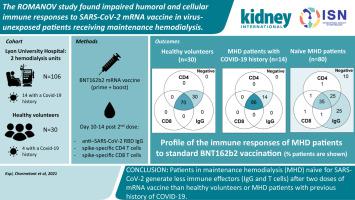
Patients on maintenance hemodialysis (MHD), which are at high risk of infection by SARS-CoV-2 virus and death due to COVID-19, have been prioritized for vaccination. However, because they were excluded from pivotal studies and have weakened immune responses, it is not known whether these patients are protected after the “standard” two doses of mRNA vaccines. To answer this, anti-spike receptor binding domain (RBD) IgG and interferon gamma-producing CD4+ and CD8+ specific-T cells were measured in the circulation 10-14 days after the second injection of BNT162b2 vaccine in 106 patients receiving MHD (14 with history of COVID-19) and compared to 30 healthy volunteers (four with history of COVID-19). After vaccination, most (72/80, 90%) patients receiving MHD naïve for the virus generated at least one type of immune effector, but their response was weaker and less complete than that of healthy volunteers. In multivariate analysis, hemodialysis and immunosuppressive therapy were significantly associated with absence of both anti-RBD IgGs and anti-spike CD8+ T cells. In contrast, previous history of COVID-19 in patients receiving MHD correlated with the generation of both types of immune effectors anti-RBD IgG and anti-spike CD8+ T cells at levels similar to healthy volunteers. Patients receiving MHD naïve for SARS-Cov-2 generate mitigated immune responses after two doses of mRNA vaccine. Thus, the good response to vaccine of patients receiving MHD with a history of COVID-19 suggest that these patients may benefit from a third vaccine injection.
中文翻译:

ROMANOV 研究发现,在接受维持性血液透析的未暴露于病毒的患者中,对 SARS-CoV-2 mRNA 疫苗的体液和细胞免疫反应受损
维持性血液透析 (MHD) 患者感染 SARS-CoV-2 病毒和因 COVID-19 死亡的风险高,已被优先接种疫苗。然而,由于他们被排除在关键研究之外并且免疫反应减弱,因此尚不清楚这些患者在“标准”两剂 mRNA 疫苗后是否受到保护。为了回答这个问题,抗尖峰受体结合域 (RBD) IgG 和产生干扰素 γ 的 CD4 +和 CD8 +106 名接受 MHD 的患者(14 名有 COVID-19 病史)在第二次注射 BNT162b2 疫苗后 10-14 天测量循环中的特异性 T 细胞,并与 30 名健康志愿者(4 名有 COVID-19 病史)进行比较。接种疫苗后,大多数(72/80,90%)接受 MHD 病毒治疗的患者至少会产生一种免疫效应物,但与健康志愿者相比,他们的反应较弱且不完全。在多变量分析中,血液透析和免疫抑制治疗与抗 RBD IgG 和抗尖峰 CD8 + T 细胞的缺失显着相关。相比之下,接受 MHD 的患者的 COVID-19 既往史与两种类型的免疫效应物抗 RBD IgG 和抗尖峰 CD8 + 的产生相关T 细胞水平与健康志愿者相似。接受 SARS-Cov-2 MHD 治疗的患者在接种两剂 mRNA 疫苗后会产生减轻的免疫反应。因此,有 COVID-19 病史的 MHD 患者对疫苗的良好反应表明这些患者可能会从第三次疫苗注射中受益。











































 京公网安备 11010802027423号
京公网安备 11010802027423号