Current HIV Research ( IF 0.8 ) Pub Date : 2021-11-30 , DOI: 10.2174/1570162x19666210625103902 Hong-Ha M Truong 1 , Robin Fatch 1 , Steven G Deeks 1 , Melissa Krone 1 , Jeffrey N Martin 1 , Peter W Hunt 1 , Paula J Lum 1
|
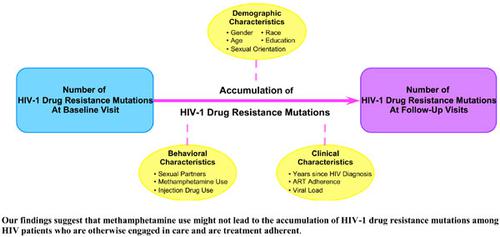
Background: Antiretroviral therapy (ART) non-adherence and methamphetamine use are associated with higher HIV drug resistance prevalence. How they affect drug resistance mutations accumulation is less studied.
Objective: We assessed factors associated with drug resistance mutations accumulation.
Methods: We evaluated HIV chronically-infected patients from a clinic-based research cohort on first-line ART regimens with genotype results within 30 days of baseline. Methamphetamine use and ART adherence were self-reported at each study visit. High ART adherence was defined as 0-5% missed doses in the last 30 days.
Results: One-hundred twenty-five patients contributed 496 study visits. At baseline, 81% of patients reported high ART adherence; 90% reported no methamphetamine use in the prior 4 months, 8% used monthly or less and 2% used daily or weekly. Methamphetamine users and non-users had similarly high ART adherence (p=0.93). Adjusted incidence rate ratio (aIRR) of drug resistance mutations accumulation was 2.04 (95% CI 0.64, 6.46) for daily/weekly users and 1.71 (95% CI 0.66, 4.42) for patients with monthly or less users, compared to non-users. aIRR was 0.71 (95% CI 0.44, 1.15) with >5-10% missed ART doses and 1.21 (95% CI 0.80, 1.83) with >10% missed doses compared to 0-5% missed doses.
Conclusion: We found no strong evidence for the effect of methamphetamine use and ART adherence on drug resistance mutations accumulation. Research cohort patients may have been more engaged in care and treatment adherent than non-cohort patients. Our findings suggest methamphetamine use might not lead to treatment failure among HIV patients who are otherwise engaged in care.
中文翻译:

HIV-1 耐药性突变的积累和甲基苯丙胺的使用
背景:抗逆转录病毒治疗 (ART) 不依从和甲基苯丙胺的使用与较高的 HIV 耐药率相关。它们如何影响耐药突变积累的研究较少。
目的:我们评估了与耐药突变积累相关的因素。
方法:我们对来自临床研究队列的 HIV 慢性感染患者进行了一线 ART 治疗方案的评估,并在基线后 30 天内获得了基因型结果。每次研究访视时都会自我报告甲基苯丙胺的使用和抗逆转录病毒治疗的依从性。高 ART 依从性定义为过去 30 天内有 0-5% 的漏服剂量。
结果:125 名患者贡献了 496 次研究访问。在基线时,81% 的患者报告说 ART 依从性很高;90% 的人表示在过去 4 个月内没有使用甲基苯丙胺,8% 的人每月或更少使用甲基苯丙胺,2% 的人每天或每周使用一次。甲基苯丙胺使用者和非使用者的 ART 依从性相似(p=0.93)。与非使用者相比,每日/每周使用者的耐药突变积累调整后发生率比 (aIRR) 为 2.04 (95% CI 0.64, 6.46),每月或更少使用者的患者为 1.71 (95% CI 0.66, 4.42) 。与 0-5% 漏服 ART 剂量相比,aIRR 为 0.71 (95% CI 0.44, 1.15),漏服剂量 > 5-10% 时;漏服剂量 > 10% 时,aIRR 为 1.21 (95% CI 0.80, 1.83)。
结论:我们没有发现强有力的证据表明甲基苯丙胺的使用和 ART 依从性对耐药突变积累的影响。研究队列患者可能比非队列患者更积极地参与护理和治疗依从性。我们的研究结果表明,使用甲基苯丙胺可能不会导致接受其他护理的艾滋病毒患者的治疗失败。











































 京公网安备 11010802027423号
京公网安备 11010802027423号