Current HIV Research ( IF 0.8 ) Pub Date : 2021-08-31 , DOI: 10.2174/1570162x19666210611145635 Eric Then 1 , Dustin J Uhlenhopp 2 , Mohamed Barakat 1 , Febin John 1 , Vijay Gayam 3 , Michell Lopez 4 , Tagore Sunkara 4 , Vinaya Gaduputi 5
|
Background: The “remission theory” is an emerging concept that suggests the presence of human immunodeficiency virus (HIV) results in decreased disease severity in patients with inflammatory bowel disease. This theory is based upon evidence that implicates CD4 T-lymphocytes in the pathogenesis of both Crohn’s disease and ulcerative colitis. This study sought to elucidate the legitimacy of this theory.
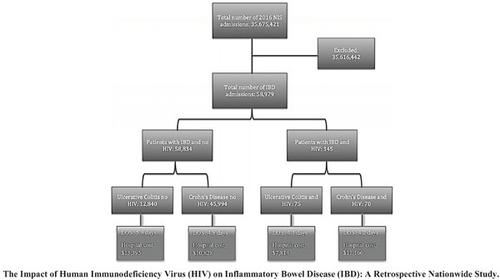
Methods: A retrospective cohort analysis of all adult inpatient hospitalizations for inflammatory bowel disease (IBD) using the 2016 National Inpatient Sample (NIS) was conducted. Our study population included patients admitted with IBD who were infected with HIV. We compared our study group to patients who also had IBD but were not infected with HIV. Baseline demographic characteristics, resource utilization, and in-hospital mortality rates were extracted for both groups.
Results: A total of 58,979 patients were admitted for IBD in 2016. Of those patients, we identified 145 who also had the presence of HIV. We found that patients with ulcerative colitis and HIV had a shorter length of hospital stay (4.1 vs. 5.9 days, p-value < 0.01), lower hospital charge ($35,716 vs $52,893, p-value < 0.01), and lower hospital cost ($7,814 vs. $13,395, p-value < 0.01) than those who did not have HIV. In patients with Crohn’s disease, the presence of HIV resulted in decreased colonoscopy rates (0% vs. 17.4%, p-value < 0.01); however, the rate of esophagogastroduodenoscopies was not statistically significant (7.1% vs. 14.7%, p-value 0.106).
Conclusion: In this retrospective population-based study, we found that patients with ulcerative colitis and concurrent HIV had a milder course of the disease when compared to ulcerative colitis patients that were not infected with HIV. These findings support the remission theory in that HIV may play a role in inflammatory bowel disease.
中文翻译:

人类免疫缺陷病毒 (HIV) 对炎症性肠病 (IBD) 的影响:一项全国性回顾性研究
背景:“缓解理论”是一个新兴概念,表明人类免疫缺陷病毒 (HIV) 的存在会降低炎症性肠病患者的疾病严重程度。该理论基于表明 CD4 T 淋巴细胞参与克罗恩病和溃疡性结肠炎发病机制的证据。本研究旨在阐明这一理论的合法性。
方法:使用 2016 年全国住院患者样本 (NIS) 对所有因炎症性肠病 (IBD) 住院的成人患者进行回顾性队列分析。我们的研究人群包括感染 HIV 的 IBD 患者。我们将我们的研究组与同样患有 IBD 但未感染 HIV 的患者进行了比较。提取了两组的基线人口统计学特征、资源利用率和住院死亡率。
结果:2016 年共有 58,979 名患者因 IBD 入院。在这些患者中,我们确定了 145 名同时存在 HIV 的患者。我们发现患有溃疡性结肠炎和 HIV 的患者住院时间更短(4.1 天 vs. 5.9 天,p 值 < 0.01),住院费用更低(35,716 美元 vs 52,893 美元,p 值 < 0.01),住院费用更低( 7,814 美元对 13,395 美元,p 值 < 0.01)比没有感染 HIV 的人高。在克罗恩病患者中,HIV 的存在导致结肠镜检查率降低(0% 对 17.4%,p 值 < 0.01);然而,食管胃十二指肠镜检查的发生率没有统计学意义(7.1% 对 14.7%,p 值 0.106)。
结论:在这项基于人群的回顾性研究中,我们发现与未感染 HIV 的溃疡性结肠炎患者相比,并发 HIV 的溃疡性结肠炎患者的病程较轻。这些发现支持缓解理论,即 HIV 可能在炎症性肠病中起作用。











































 京公网安备 11010802027423号
京公网安备 11010802027423号