当前位置:
X-MOL 学术
›
Brain Pathol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
COVID-19-related neuropathology and microglial activation in elderly with and without dementia
Brain Pathology ( IF 5.8 ) Pub Date : 2021-06-18 , DOI: 10.1111/bpa.12997 Tino Emanuele Poloni 1, 2 , Valentina Medici 1 , Matteo Moretti 3 , Silvia Damiana Visonà 3 , Alice Cirrincione 1 , Arenn Faye Carlos 1 , Annalisa Davin 1 , Stella Gagliardi 4 , Orietta Pansarasa 4 , Cristina Cereda 4 , Livio Tronconi 3, 5 , Antonio Guaita 1 , Mauro Ceroni 6, 7
Brain Pathology ( IF 5.8 ) Pub Date : 2021-06-18 , DOI: 10.1111/bpa.12997 Tino Emanuele Poloni 1, 2 , Valentina Medici 1 , Matteo Moretti 3 , Silvia Damiana Visonà 3 , Alice Cirrincione 1 , Arenn Faye Carlos 1 , Annalisa Davin 1 , Stella Gagliardi 4 , Orietta Pansarasa 4 , Cristina Cereda 4 , Livio Tronconi 3, 5 , Antonio Guaita 1 , Mauro Ceroni 6, 7
Affiliation
|
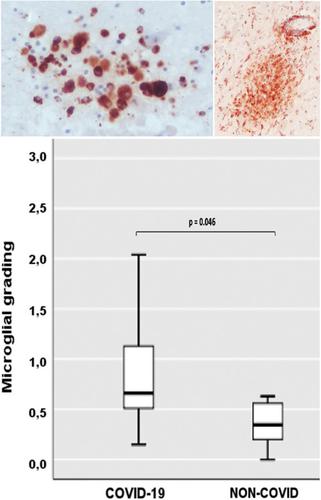
The actual role of SARS-CoV-2 in brain damage remains controversial due to lack of matched controls. We aim to highlight to what extent is neuropathology determined by SARS-CoV-2 or by pre-existing conditions. Findings of 9 Coronavirus disease 2019 (COVID-19) cases and 6 matched non-COVID controls (mean age 79 y/o) were compared. Brains were analyzed through immunohistochemistry to detect SARS-CoV-2, lymphocytes, astrocytes, endothelium, and microglia. A semi-quantitative scoring was applied to grade microglial activation. Thal-Braak stages and the presence of small vessel disease were determined in all cases. COVID-19 cases had a relatively short clinical course (0–32 days; mean: 10 days), and did not undergo mechanical ventilation. Five patients with neurocognitive disorder had delirium. All COVID-19 cases showed non-SARS-CoV-2-specific changes including hypoxic-agonal alterations, and a variable degree of neurodegeneration and/or pre-existent SVD. The neuroinflammatory picture was dominated by ameboid CD68 positive microglia, while only scant lymphocytic presence and very few traces of SARS-CoV-2 were detected. Microglial activation in the brainstem was significantly greater in COVID-19 cases (p = 0.046). Instead, microglial hyperactivation in the frontal cortex and hippocampus was clearly associated to AD pathology (p = 0.001), regardless of the SARS-CoV-2 infection. In COVID-19 cases complicated by delirium (all with neurocognitive disorders), there was a significant enhancement of microglia in the hippocampus (p = 0.048). Although higher in cases with both Alzheimer's pathology and COVID-19, cortical neuroinflammation is not related to COVID-19 per se but mostly to pre-existing neurodegeneration. COVID-19 brains seem to manifest a boosting of innate immunity with microglial reinforcement, and adaptive immunity suppression with low number of brain lymphocytes probably related to systemic lymphopenia. Thus, no neuropathological evidence of SARS-CoV-2-specific encephalitis is detectable. The microglial hyperactivation in the brainstem, and in the hippocampus of COVID-19 patients with delirium, appears as a specific topographical phenomenon, and probably represents the neuropathological basis of the “COVID-19 encephalopathic syndrome” in the elderly.
中文翻译:

患有或不患有痴呆症的老年人中与 COVID-19 相关的神经病理学和小胶质细胞激活
由于缺乏匹配的对照,SARS-CoV-2 在脑损伤中的实际作用仍然存在争议。我们的目的是强调神经病理学在多大程度上是由 SARS-CoV-2 或既往病症决定的。对 9 例 2019 年冠状病毒病 (COVID-19) 病例和 6 例匹配的非 COVID 对照(平均年龄 79 岁)的结果进行了比较。通过免疫组织化学对大脑进行分析,以检测 SARS-CoV-2、淋巴细胞、星形胶质细胞、内皮细胞和小胶质细胞。应用半定量评分对小胶质细胞激活进行分级。在所有病例中均确定了 Thal-Braak 分期和小血管疾病的存在。COVID-19病例的临床病程相对较短(0-32天;平均:10天),并且未接受机械通气。5名神经认知障碍患者出现 谵妄。所有 COVID-19 病例均表现出非 SARS-CoV-2 特异性变化,包括缺氧激动改变以及不同程度的神经变性和/或预先存在的 SVD。神经炎症图像以阿米巴 CD68 阳性小胶质细胞为主,而仅检测到少量淋巴细胞和极少数 SARS-CoV-2 痕迹。在 COVID-19 病例中,脑干中的小胶质细胞激活显着增强 ( p = 0.046)。 相反,无论是否感染 SARS-CoV-2,额叶皮层和海马区的小胶质细胞过度激活与 AD 病理学明显相关 ( p = 0.001)。在并发谵妄的 COVID-19 病例中(均伴有神经认知障碍),海马中的小胶质细胞显着增强 ( p = 0.048)。尽管在同时患有阿尔茨海默病和 COVID-19 的病例中皮质神经炎症较高,但皮质神经炎症与 COVID-19本身无关,而主要与先前存在的神经变性有关。COVID-19 大脑似乎表现出通过小胶质细胞强化增强先天免疫,以及通过低数量脑淋巴细胞抑制适应性免疫,这可能与全身性淋巴细胞减少有关。因此,没有检测到 SARS-CoV-2 特异性脑炎的神经病理学证据。患有谵妄的COVID-19患者脑干和海马中的小胶质细胞过度活跃,表现为一种特定的拓扑现象,可能代表了老年人“COVID-19脑病综合征”的神经病理学基础。
更新日期:2021-08-25
中文翻译:

患有或不患有痴呆症的老年人中与 COVID-19 相关的神经病理学和小胶质细胞激活
由于缺乏匹配的对照,SARS-CoV-2 在脑损伤中的实际作用仍然存在争议。我们的目的是强调神经病理学在多大程度上是由 SARS-CoV-2 或既往病症决定的。对 9 例 2019 年冠状病毒病 (COVID-19) 病例和 6 例匹配的非 COVID 对照(平均年龄 79 岁)的结果进行了比较。通过免疫组织化学对大脑进行分析,以检测 SARS-CoV-2、淋巴细胞、星形胶质细胞、内皮细胞和小胶质细胞。应用半定量评分对小胶质细胞激活进行分级。在所有病例中均确定了 Thal-Braak 分期和小血管疾病的存在。COVID-19病例的临床病程相对较短(0-32天;平均:10天),并且未接受机械通气。5名神经认知障碍患者出现 谵妄。所有 COVID-19 病例均表现出非 SARS-CoV-2 特异性变化,包括缺氧激动改变以及不同程度的神经变性和/或预先存在的 SVD。神经炎症图像以阿米巴 CD68 阳性小胶质细胞为主,而仅检测到少量淋巴细胞和极少数 SARS-CoV-2 痕迹。在 COVID-19 病例中,脑干中的小胶质细胞激活显着增强 ( p = 0.046)。 相反,无论是否感染 SARS-CoV-2,额叶皮层和海马区的小胶质细胞过度激活与 AD 病理学明显相关 ( p = 0.001)。在并发谵妄的 COVID-19 病例中(均伴有神经认知障碍),海马中的小胶质细胞显着增强 ( p = 0.048)。尽管在同时患有阿尔茨海默病和 COVID-19 的病例中皮质神经炎症较高,但皮质神经炎症与 COVID-19本身无关,而主要与先前存在的神经变性有关。COVID-19 大脑似乎表现出通过小胶质细胞强化增强先天免疫,以及通过低数量脑淋巴细胞抑制适应性免疫,这可能与全身性淋巴细胞减少有关。因此,没有检测到 SARS-CoV-2 特异性脑炎的神经病理学证据。患有谵妄的COVID-19患者脑干和海马中的小胶质细胞过度活跃,表现为一种特定的拓扑现象,可能代表了老年人“COVID-19脑病综合征”的神经病理学基础。











































 京公网安备 11010802027423号
京公网安备 11010802027423号