当前位置:
X-MOL 学术
›
J. Am. Coll. Cardiol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Aortic Valve Replacement in Low-Risk Patients With Severe Aortic Stenosis Outside Randomized Trials
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2021-01-01 , DOI: 10.1016/j.jacc.2020.10.056 Alberto Alperi 1 , Pierre Voisine 1 , Dimitri Kalavrouziotis 1 , Eric Dumont 1 , François Dagenais 1 , Jean Perron 1 , Iria Silva 1 , Fernando Bernardi 1 , Siamak Mohammadi 1 , Josep Rodés-Cabau 1
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2021-01-01 , DOI: 10.1016/j.jacc.2020.10.056 Alberto Alperi 1 , Pierre Voisine 1 , Dimitri Kalavrouziotis 1 , Eric Dumont 1 , François Dagenais 1 , Jean Perron 1 , Iria Silva 1 , Fernando Bernardi 1 , Siamak Mohammadi 1 , Josep Rodés-Cabau 1
Affiliation
|
BACKGROUND
Recent randomized trials including low-risk patients showed positive results for transcatheter aortic valve replacement (TAVR) compared to surgical aortic valve replacement (SAVR), but patients with non-tricuspid aortic valve (NTAV), severe coronary artery disease (SevCAD), and those requiring concomitant mitral/tricuspid valve (CMTV) or concomitant ascending aorta replacement (CAAR) interventions were excluded. OBJECTIVES
This study sought to evaluate the presence and impact of the main clinical variables not evaluated in TAVR versus SAVR trials (NTAV, SevCAD, and CMTV or CAAR intervention) in a large series of consecutive low-risk patients with severe aortic stenosis (SAS) undergoing SAVR. METHODS
Single-center study including consecutive patients with SAS and low surgical risk (Society of Thoracic Surgeons score of <4%) undergoing SAVR. Baseline, procedural characteristics, and 30-day outcomes were prospectively collected. RESULTS
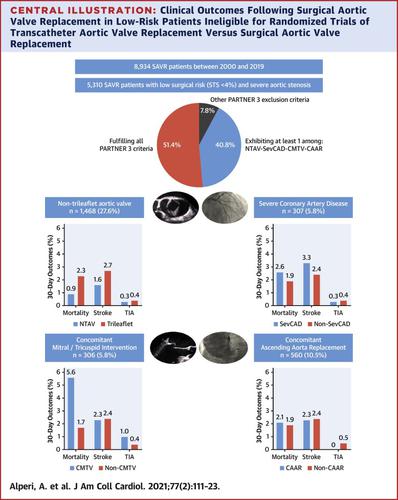
Of 6,772 patients with SAS who underwent SAVR between 2000 and 2019, 5,310 (78.4%) exhibited a low surgical risk (mean Society of Thoracic Surgeons score: 1.94 ± 0.87%). Of these, 2,165 patients (40.8%) had at least 1 of the following: NTAV (n = 1,468, 27.6%), SevCAD (n = 307, 5.8%), CMTV (n = 306, 5.8%), and CAAR (n = 560, 10.5%). The 30-day mortality and stroke rates for the overall low-risk SAS cohort were 1.9% and 2.4%, respectively. The mortality rate was similar in the SevCAD (2.6%) and CAAR (2.1%) groups versus the rest of the cohort (odds ratio [OR]: 1.79; 95% confidence interval [CI]: 0.85 to 3.75, and OR: 1.64; 95% CI: 0.88 to 3.05, respectively), lower in the NTAV group (0.9%; OR: 0.42; 95% CI: 0.22 to 0.81), and higher in the CMTV group (5.9%; OR: 2.61; 95% CI: 1.51 to 4.5). CONCLUSIONS
In a real-world setting, close to one-half of the low-risk patients with SAS undergoing SAVR exhibited at least 1 major criterion not evaluated in TAVR versus SAVR randomized trials. Clinical outcomes were better than or similar to those predicted by surgical scores in all groups but those patients requiring CMTV intervention. These results may help determine the impact of implementing the results of TAVR-SAVR trials in real practice and may inform future trials in specific groups.
中文翻译:

随机试验之外重度主动脉瓣狭窄低风险患者的主动脉瓣置换术
背景 最近包括低风险患者在内的随机试验显示,与外科主动脉瓣置换术 (SAVR) 相比,经导管主动脉瓣置换术 (TAVR) 的阳性结果,但非三尖瓣主动脉瓣 (NTAV)、严重冠状动脉疾病 (SevCAD)、那些需要伴随二尖瓣/三尖瓣(CMTV)或伴随升主动脉置换(CAAR)干预的患者被排除在外。目的 本研究旨在评估 TAVR 与 SAVR 试验(NTAV、SevCAD 和 CMTV 或 CAAR 干预)中未评估的主要临床变量的存在和影响,这些变量在一系列连续的严重主动脉瓣狭窄 (SAS) 低风险患者中进行正在经历 SAVR。方法 单中心研究包括 SAS 和低手术风险的连续患者(胸外科医师协会评分 < 4%) 正在经历 SAVR。前瞻性收集基线、程序特征和 30 天结果。结果 在 2000 年至 2019 年间接受 SAVR 的 6,772 名 SAS 患者中,5,310 名 (78.4%) 的手术风险较低(平均胸外科医师协会评分:1.94 ± 0.87%)。其中,2,165 名患者 (40.8%) 至少有以下一项:NTAV (n = 1,468, 27.6%)、SevCAD (n = 307, 5.8%)、CMTV (n = 306, 5.8%) 和 CAAR ( n = 560, 10.5%)。整个低风险 SAS 队列的 30 天死亡率和卒中率分别为 1.9% 和 2.4%。SevCAD (2.6%) 和 CAAR (2.1%) 组与其他队列的死亡率相似(优势比 [OR]:1.79;95% 置信区间 [CI]:0.85 至 3.75,OR:1.64 ;95% CI:分别为 0.88 至 3.05),在 NTAV 组中较低(0.9%;OR:0.42;95% CI:0.22 至 0.81),CMTV 组更高(5.9%;OR:2.61;95% CI:1.51 至 4.5)。结论 在现实世界中,接近一半的 SAS 接受 SAVR 的低风险患者表现出至少 1 个未在 TAVR 与 SAVR 随机试验中评估的主要标准。除需要 CMTV 干预的患者外,所有组的临床结果均优于或类似于手术评分预测的结果。这些结果可能有助于确定在实际实践中实施 TAVR-SAVR 试验结果的影响,并可能为特定群体的未来试验提供信息。除需要 CMTV 干预的患者外,所有组的临床结果均优于或类似于手术评分预测的结果。这些结果可能有助于确定在实际实践中实施 TAVR-SAVR 试验结果的影响,并可能为特定群体的未来试验提供信息。除需要 CMTV 干预的患者外,所有组的临床结果均优于或类似于手术评分预测的结果。这些结果可能有助于确定在实际实践中实施 TAVR-SAVR 试验结果的影响,并可能为特定群体的未来试验提供信息。
更新日期:2021-01-01
中文翻译:

随机试验之外重度主动脉瓣狭窄低风险患者的主动脉瓣置换术
背景 最近包括低风险患者在内的随机试验显示,与外科主动脉瓣置换术 (SAVR) 相比,经导管主动脉瓣置换术 (TAVR) 的阳性结果,但非三尖瓣主动脉瓣 (NTAV)、严重冠状动脉疾病 (SevCAD)、那些需要伴随二尖瓣/三尖瓣(CMTV)或伴随升主动脉置换(CAAR)干预的患者被排除在外。目的 本研究旨在评估 TAVR 与 SAVR 试验(NTAV、SevCAD 和 CMTV 或 CAAR 干预)中未评估的主要临床变量的存在和影响,这些变量在一系列连续的严重主动脉瓣狭窄 (SAS) 低风险患者中进行正在经历 SAVR。方法 单中心研究包括 SAS 和低手术风险的连续患者(胸外科医师协会评分 < 4%) 正在经历 SAVR。前瞻性收集基线、程序特征和 30 天结果。结果 在 2000 年至 2019 年间接受 SAVR 的 6,772 名 SAS 患者中,5,310 名 (78.4%) 的手术风险较低(平均胸外科医师协会评分:1.94 ± 0.87%)。其中,2,165 名患者 (40.8%) 至少有以下一项:NTAV (n = 1,468, 27.6%)、SevCAD (n = 307, 5.8%)、CMTV (n = 306, 5.8%) 和 CAAR ( n = 560, 10.5%)。整个低风险 SAS 队列的 30 天死亡率和卒中率分别为 1.9% 和 2.4%。SevCAD (2.6%) 和 CAAR (2.1%) 组与其他队列的死亡率相似(优势比 [OR]:1.79;95% 置信区间 [CI]:0.85 至 3.75,OR:1.64 ;95% CI:分别为 0.88 至 3.05),在 NTAV 组中较低(0.9%;OR:0.42;95% CI:0.22 至 0.81),CMTV 组更高(5.9%;OR:2.61;95% CI:1.51 至 4.5)。结论 在现实世界中,接近一半的 SAS 接受 SAVR 的低风险患者表现出至少 1 个未在 TAVR 与 SAVR 随机试验中评估的主要标准。除需要 CMTV 干预的患者外,所有组的临床结果均优于或类似于手术评分预测的结果。这些结果可能有助于确定在实际实践中实施 TAVR-SAVR 试验结果的影响,并可能为特定群体的未来试验提供信息。除需要 CMTV 干预的患者外,所有组的临床结果均优于或类似于手术评分预测的结果。这些结果可能有助于确定在实际实践中实施 TAVR-SAVR 试验结果的影响,并可能为特定群体的未来试验提供信息。除需要 CMTV 干预的患者外,所有组的临床结果均优于或类似于手术评分预测的结果。这些结果可能有助于确定在实际实践中实施 TAVR-SAVR 试验结果的影响,并可能为特定群体的未来试验提供信息。











































 京公网安备 11010802027423号
京公网安备 11010802027423号