Experimental Cell Research ( IF 3.3 ) Pub Date : 2021-01-08 , DOI: 10.1016/j.yexcr.2021.112473 Amir K. Varkouhi , Xiaolin He , Ana Paula Teixeira Monteiro , Hajera Amatullah , James N. Tsoporis , Sahil Gupta , Amin M. Ektesabi , Shirley H.J. Mei , Duncan J. Stewart , Armand Keating , Claudia C. dos Santos
|
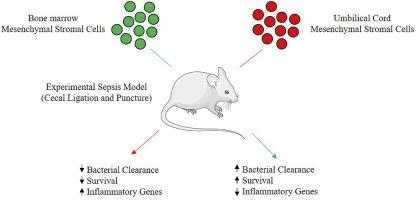
Sepsis is a complicated multi-system disorder characterized by a dysregulated host response to infection. Despite substantial progress in the understanding of mechanisms of sepsis, translation of these advances into clinically effective therapies remains challenging. Mesenchymal Stromal Cells (MSCs) possess immunomodulatory properties that have shown therapeutic promise in preclinical models of sepsis. The therapeutic effects of MSCs may vary depending on the source and type of these cells. In this comparative study, the gene expression pattern and surface markers of bone marrow-derived MSCs (BM-MSCs) and umbilical cord-derived MSCs (UC-MSCs) as well as their therapeutic effects in a clinically relevant mouse model of polymicrobial sepsis, cecal ligation and puncture (CLP), were investigated. The results showed remarkable differences in gene expression profile, surface markers and therapeutic potency in terms of enhancing survival and pro/anti-inflammatory responses between the two MSC types. BM-MSCs improved survival concomitant with an enhanced systemic bacterial clearance and improved inflammatory profile post CLP surgery. Despite some improvement in the inflammatory profile of the septic animals, treatment with UC-MSCs did not enhance survival or bacterial clearance. Overall, the beneficial therapeutic effects of BM-MSCs over UC-MSCs may likely be attributed to their pro-inflammatory function, and to some extent anti-inflammatory features, reflected in their gene expression pattern enhancing macrophage polarization to M1/M2 phenotypes resulting in a balanced pro- and anti-inflammatory response against polymicrobial sepsis.
中文翻译:

脓毒症实验模型中人骨髓和脐带间充质基质细胞的免疫表型表征和治疗作用
脓毒症是一种复杂的多系统疾病,其特征在于宿主对感染的反应失调。尽管在对败血症机制的理解上取得了重大进展,但是将这些进展转化为临床有效的疗法仍然具有挑战性。间质基质细胞(MSC)具有免疫调节特性,在脓毒症的临床前模型中显示出治疗前景。MSC的治疗效果可能取决于这些细胞的来源和类型。在这项比较研究中,骨髓来源的MSCs(BM-MSCs)和脐带来源的MSCs(UC-MSCs)的基因表达模式和表面标记,以及它们在临床上相关的多菌血症小鼠模型中的治疗作用,盲肠结扎和穿刺(CLP),进行了调查。结果显示,就两种MSC类型而言,在提高存活率和促炎/抗炎反应方面,基因表达谱,表面标志物和治疗效力存在显着差异。BM-MSC在CLP手术后改善了生存率,同时增强了系统性细菌清除率并改善了炎症状况。尽管脓毒症动物的炎症特征有所改善,但使用UC-MSC的治疗并未提高存活率或细菌清除率。总体而言,BM-MSC对UC-MSC的有益治疗作用可能归因于其促炎功能,并在一定程度上具有抗炎特性,体现在它们的基因表达模式中,使巨噬细胞极化增强为M1 / M2表型,从而导致针对多菌血症的平衡的促炎和抗炎反应。









































 京公网安备 11010802027423号
京公网安备 11010802027423号