International Journal for Parasitology ( IF 3.7 ) Pub Date : 2020-12-24 , DOI: 10.1016/j.ijpara.2020.10.001 Adeyemi T Kayode 1 , Kazeem Akano 1 , Fehintola V Ajogbasile 1 , Jessica N Uwanibe 1 , Paul E Oluniyi 1 , Bolajoko E Bankole 1 , Philomena J Eromon 2 , Akintunde Sowunmi 3 , Onikepe A Folarin 1 , Sarah K Volkman 4 , Bronwyn McInnis 5 , Pardis Sabeti 4 , Dyann F Wirth 4 , Christian T Happi 6
|
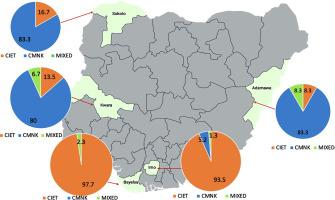
The emergence and spread of Plasmodium falciparum parasites resistant to artemisinin derivatives and their partners in southeastern Asia threatens malaria control and elimination efforts, and heightens the need for an alternative therapy. We have explored the distribution of P. falciparum chloroquine resistance transporter (Pfcrt) and multidrug-resistant gene 1 (Pfmdr-1) haplotypes 10 years following adoption of artemisinin-based combination therapies in a bid to investigate the possible re-emergence of Chloroquine-sensitive parasites in Nigeria, and investigated the effect of these P. falciparum haplotypes on treatment outcomes of patients treated with artemisinin-based combination therapies. A total of 271 children aged <5 years with uncomplicated falciparum malaria were included in this study. Polymorphisms on codons 72–76 of the Pfcrt gene and codon 86 and 184 of Pfmdr-1 were determined using the high resolution melting assay. Of 240 (88.6%) samples successfully genotyped with HRM for Pfcrt, wildtype C72M74N75K76 (42.9%) and mutant C72I74E75T76 (53.8%) were observed. Also, wildtype N86Y184 (62.9%) and mutant N86F184 (21.1%), Y86Y184 (6.4%), and Y86F184 (0.4%) haplotypes of Pfmdr-1 were observed. Measures of responsiveness to ACTs were similar in children infected with P. falciparum crt haplotypes (C72I74E75T76 and C72M74N75K76) and major mdr-1 haplotypes (N86Y184, N86F184 and Y86Y184). Despite a 10 year gap since the malaria treatment policy changed to ACTs, over 50% of the P. falciparum parasites investigated in this study harboured the Chloroquine-resistant C72I74E75T76 haplotype, however this did not compromise the efficacy of artemisinin-based combination therapies. Should complete artemisinin resistance emerge from or spread to Nigeria, chloroquine might not be a good alternative therapy.
中文翻译:

采用青蒿素联合治疗 10 年后,尼日利亚儿童恶性疟原虫氯喹耐药转运蛋白 (Pfcrt) 和多重耐药基因 1 (Pfmdr-1) 的多态性
对青蒿素衍生物及其伙伴具有抗药性的恶性疟原虫在东南亚的出现和传播威胁着疟疾的控制和消除工作,并增加了对替代疗法的需求。我们探索了采用基于青蒿素的联合疗法 10 年后恶性疟原虫氯喹耐药转运蛋白 ( Pfcrt ) 和多重耐药基因 1 ( Pfmdr- 1 ) 单倍型的分布,以调查氯喹是否可能重新出现。尼日利亚的敏感寄生虫,并研究了这些恶性疟原虫单倍型对接受基于青蒿素的联合疗法的患者的治疗结果的影响。使用高分辨率解链测定法测定了总共271名<5岁儿童的Pfcrt基因和Pfmdr -1的密码子86和184。在 240 个 (88.6%) 样本中成功使用 HRM 进行Pfcrt基因分型,观察到野生型 C 72 M 74 N 75 K 76 (42.9%) 和突变型 C 72 I 74 E 75 T 76 (53.8%)。此外,还观察到Pfmdr -1 的野生型N 86 Y 184 (62.9%)和突变型N 86 F 184 (21.1%)、Y 86 Y 184 (6.4%)和Y 86 F 184 (0.4%)单倍型。感染P 的儿童对 ACT 的反应性测量相似。 恶性疟 crt 单倍型(C 72 I 74 E 75 T 76和 C 72 M 74 N 75 K 76 )和主要mdr -1 单倍型(N 86 Y 184 、N 86 F 184和 Y 86 Y 184 )。尽管自疟疾治疗政策改为 ACT 以来已有 10 年的时间间隔,但本研究中调查的恶性疟原虫寄生虫中超过 50% 含有氯喹抗性 C 72 I 74 E 75 T 76单倍型,但这并没有影响 ACT 的疗效。以青蒿素为基础的联合疗法。如果尼日利亚出现或蔓延到青蒿素完全耐药性,氯喹可能不是一个好的替代疗法。










































 京公网安备 11010802027423号
京公网安备 11010802027423号