当前位置:
X-MOL 学术
›
J. Cyst. Fibros.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
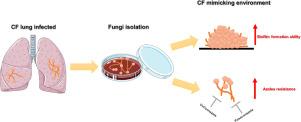
Impact of biofilm formation and azoles' susceptibility in Scedosporium/Lomentospora species using an in vitro model that mimics the cystic fibrosis patients' airway environment
Journal of Cystic Fibrosis ( IF 5.4 ) Pub Date : 2020-12-01 , DOI: 10.1016/j.jcf.2020.12.001 Thaís P Mello 1 , Michaela Lackner 2 , Marta H Branquinha 1 , André L S Santos 3
Journal of Cystic Fibrosis ( IF 5.4 ) Pub Date : 2020-12-01 , DOI: 10.1016/j.jcf.2020.12.001 Thaís P Mello 1 , Michaela Lackner 2 , Marta H Branquinha 1 , André L S Santos 3
Affiliation
|
BACKGROUND
Scedosporium species are the second most isolated filamentous fungi from cystic fibrosis (CF) patients; however, little is known about their virulence aspects in a CF environment. In this context, the current study aimed to evaluate the (i) antifungal susceptibility profiles, (ii) ability to form biofilm and (iii) impact of biofilm formation on the susceptibility to azoles in 21 clinical isolates of Scedosporium recovered from CF patients. METHODS
Scedosporium apiospermum (n=6), S. aurantiacum (n=6), S. minutisporum (n=3) and Lomentospora prolificans (n=6) were firstly used to compare the antifungal susceptibility profile using a standard culture broth (RPMI-1640) and a mucin (M)-containing synthetic CF sputum medium (SCFM). The ability to form biofilms was investigated in polystyrene microtiter plates containing Sabouraud-dextrose (a classical medium), SCFM and SCFM+M. Mature biofilms were tested for their susceptibility to azoles by microdilution assay. RESULTS
Our results showed that the minimum inhibitory concentrations (MICs) for planktonic conidia ranged from 0.25 to >16.0 mg/L for voriconazole and 1.0 to >16.0 mg/L for posaconazole. Overall, the MICs for azoles increased from 2- to 8-folds when the susceptibility tests were performed using SCFM+M compared to RPMI-1640. All fungi formed robust biofilms on polystyrene surface at 72 h, with a significant increase in the MICs (ranging from 128- to 1024-times) against both azoles compared to the planktonic cells. CONCLUSION
These findings confirm the challenge of antifungal treatment of CF patients infected with Scedosporium/Lomentospora and also demonstrated a strong biofilm formation, with extensive increase in antifungal resistance, triggered underconditions mimicking the CF patient airway.
中文翻译:

使用模拟囊性纤维化患者气道环境的体外模型对 Scedosporium/Lomentospora 物种中生物膜形成和唑类易感性的影响
背景 Scedosporium 是从囊性纤维化 (CF) 患者中分离出来的第二大丝状真菌。然而,人们对它们在 CF 环境中的毒力方面知之甚少。在这种情况下,目前的研究旨在评估(i)抗真菌敏感性曲线,(ii)形成生物膜的能力和(iii)生物膜形成对从 CF 患者中回收的 21 种临床分离的 Scedosporium 中唑类药物敏感性的影响。方法 首先使用 Scedosporium apiospermum (n=6)、S. aurantiacum (n=6)、S. minutisporum (n=3) 和 Lomentospora prolificans (n=6) 比较标准培养液 (RPMI) 的抗真菌敏感性曲线-1640) 和含有粘蛋白 (M) 的合成 CF 痰液培养基 (SCFM)。在含有沙氏葡萄糖(一种经典培养基)、SCFM 和 SCFM+M 的聚苯乙烯微量滴定板中研究了形成生物膜的能力。通过微量稀释法测试成熟生物膜对唑类的敏感性。结果 我们的结果表明,伏立康唑对浮游分生孢子的最低抑菌浓度 (MIC) 范围为 0.25 至 >16.0 mg/L,泊沙康唑为 1.0 至 >16.0 mg/L。总体而言,与 RPMI-1640 相比,使用 SCFM+M 进行敏感性测试时,唑类的 MIC 从 2 倍增加到 8 倍。与浮游细胞相比,所有真菌在聚苯乙烯表面上形成坚固的生物膜 72 小时,对两种唑类的 MIC 显着增加(从 128 到 1024 倍)。
更新日期:2020-12-01
中文翻译:

使用模拟囊性纤维化患者气道环境的体外模型对 Scedosporium/Lomentospora 物种中生物膜形成和唑类易感性的影响
背景 Scedosporium 是从囊性纤维化 (CF) 患者中分离出来的第二大丝状真菌。然而,人们对它们在 CF 环境中的毒力方面知之甚少。在这种情况下,目前的研究旨在评估(i)抗真菌敏感性曲线,(ii)形成生物膜的能力和(iii)生物膜形成对从 CF 患者中回收的 21 种临床分离的 Scedosporium 中唑类药物敏感性的影响。方法 首先使用 Scedosporium apiospermum (n=6)、S. aurantiacum (n=6)、S. minutisporum (n=3) 和 Lomentospora prolificans (n=6) 比较标准培养液 (RPMI) 的抗真菌敏感性曲线-1640) 和含有粘蛋白 (M) 的合成 CF 痰液培养基 (SCFM)。在含有沙氏葡萄糖(一种经典培养基)、SCFM 和 SCFM+M 的聚苯乙烯微量滴定板中研究了形成生物膜的能力。通过微量稀释法测试成熟生物膜对唑类的敏感性。结果 我们的结果表明,伏立康唑对浮游分生孢子的最低抑菌浓度 (MIC) 范围为 0.25 至 >16.0 mg/L,泊沙康唑为 1.0 至 >16.0 mg/L。总体而言,与 RPMI-1640 相比,使用 SCFM+M 进行敏感性测试时,唑类的 MIC 从 2 倍增加到 8 倍。与浮游细胞相比,所有真菌在聚苯乙烯表面上形成坚固的生物膜 72 小时,对两种唑类的 MIC 显着增加(从 128 到 1024 倍)。











































 京公网安备 11010802027423号
京公网安备 11010802027423号