Journal of Allergy and Clinical Immunology ( IF 11.4 ) Pub Date : 2020-11-13 , DOI: 10.1016/j.jaci.2020.11.002 Yoshihiko Raita 1 , Carlos A Camargo 1 , Yury A Bochkov 2 , Juan C Celedón 3 , James E Gern 4 , Jonathan M Mansbach 5 , Eugene P Rhee 6 , Robert J Freishtat 7 , Kohei Hasegawa 1
|
Background
Young children with rhinovirus (RV) infection—particularly bronchiolitis—are at high risk for developing childhood asthma. Emerging evidence suggests clinical heterogeneity within RV bronchiolitis. However, little is known about these biologically distinct subgroups (endotypes) and their relations with asthma risk.
Objective
We aimed to identify RV bronchiolitis endotypes and examine their longitudinal relations with asthma risk.
Methods
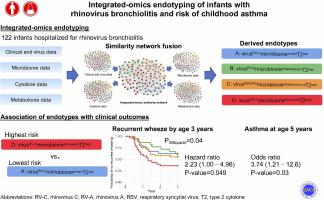
As part of a multicenter prospective cohort study of infants (age <12 months) hospitalized for bronchiolitis, we integrated clinical, RV species (RV-A, RV-B, and RV-C), nasopharyngeal microbiome (16S rRNA gene sequencing), cytokine, and metabolome (liquid chromatography tandem mass spectrometry) data collected at hospitalization. We then applied network and clustering approaches to identify bronchiolitis endotypes. We also examined their longitudinal association with risks of developing recurrent wheeze by age 3 years and asthma by age 5 years.
Results
Of 122 infants hospitalized for RV bronchiolitis (median age, 4 months), we identified 4 distinct endotypes—mainly characterized by RV species, microbiome, and type 2 cytokine (T2) response: endotype A, virusRV-CmicrobiomemixedT2low; endotype B, virusRV-AmicrobiomeHaemophilusT2low; endotype C, virusRSV/RVmicrobiomeStreptococcusT2low; and endotype D, virusRV-CmicrobiomeMoraxellaT2high. Compared with endotype A infants, endotype D infants had a significantly higher rate of recurrent wheeze (33% vs 64%; hazard ratio, 2.23; 95% CI, 1.00-4.96; P = .049) and a higher risk for developing asthma (28% vs 59%; odds ratio, 3.74: 95% CI, 1.21-12.6; P = .03).
Conclusions
Integrated-omics analysis identified biologically meaningful RV bronchiolitis endotypes in infants, such as one characterized by RV-C infection, Moraxella-dominant microbiota, and high T2 cytokine response, at higher risk for developing recurrent wheeze and asthma. This study should facilitate further research toward validating our inferences.
中文翻译:

鼻病毒性细支气管炎婴儿的综合组学内分型与儿童哮喘风险
背景
患有鼻病毒 (RV) 感染(尤其是细支气管炎)的幼儿患儿童哮喘的风险很高。新出现的证据表明 RV 细支气管炎的临床异质性。然而,对于这些生物学上不同的亚组(内型)及其与哮喘风险的关系知之甚少。
客观的
我们旨在确定 RV 细支气管炎内型并检查它们与哮喘风险的纵向关系。
方法
作为一项针对因毛细支气管炎住院的婴儿(<12 个月)的多中心前瞻性队列研究的一部分,我们整合了临床、RV 种类(RV-A、RV-B 和 RV-C)、鼻咽微生物组(16S rRNA 基因测序)、住院期间收集的细胞因子和代谢组(液相色谱串联质谱)数据。然后,我们应用网络和聚类方法来识别细支气管炎内型。我们还检查了它们与 3 岁时复发性喘息和 5 岁时发生哮喘风险的纵向关联。
结果
在 122 名因 RV 细支气管炎住院的婴儿(中位年龄 4 个月)中,我们确定了 4 种不同的内型——主要以 RV 种类、微生物组和 2 型细胞因子 (T2) 反应为特征:内型 A、病毒RV-C微生物组混合T2低;内型 B,病毒RV-A微生物组Haemophilus T2低;内型 C,病毒RSV/RV微生物组链球菌T2低;和内型 D,病毒RV-C微生物组Moraxella T2高. 与内型 A 婴儿相比,内型 D 婴儿的喘息复发率显着更高(33% 对 64%;风险比,2.23;95% CI,1.00-4.96;P = 0.049)和发生哮喘的更高风险( 28% 对 59%;优势比,3.74:95% CI,1.21-12.6;P = .03)。
结论
综合组学分析确定了婴儿中具有生物学意义的 RV 细支气管炎内型,例如以 RV-C 感染、以莫拉菌属为主的微生物群和高 T2 细胞因子反应为特征的婴儿,其发生复发性喘息和哮喘的风险较高。这项研究应该有助于进一步研究以验证我们的推论。











































 京公网安备 11010802027423号
京公网安备 11010802027423号