当前位置:
X-MOL 学术
›
J. Aerosol Sci.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Breath-, air- and surface-borne SARS-CoV-2 in hospitals
Journal of Aerosol Science ( IF 3.9 ) Pub Date : 2021-02-01 , DOI: 10.1016/j.jaerosci.2020.105693 Lian Zhou 1 , Maosheng Yao 2 , Xiang Zhang 3 , Bicheng Hu 4 , Xinyue Li 2 , Haoxuan Chen 2 , Lu Zhang 2 , Yun Liu 3 , Meng Du 5 , Bochao Sun 6 , Yunyu Jiang 7 , Kai Zhou 8 , Jie Hong 1 , Na Yu 9 , Zhen Ding 1 , Yan Xu 1 , Min Hu 2 , Lidia Morawska 10 , Sergey A Grinshpun 11 , Pratim Biswas 12 , Richard C Flagan 13 , Baoli Zhu 1, 14 , Wenqing Liu 15 , Yuanhang Zhang 2
Journal of Aerosol Science ( IF 3.9 ) Pub Date : 2021-02-01 , DOI: 10.1016/j.jaerosci.2020.105693 Lian Zhou 1 , Maosheng Yao 2 , Xiang Zhang 3 , Bicheng Hu 4 , Xinyue Li 2 , Haoxuan Chen 2 , Lu Zhang 2 , Yun Liu 3 , Meng Du 5 , Bochao Sun 6 , Yunyu Jiang 7 , Kai Zhou 8 , Jie Hong 1 , Na Yu 9 , Zhen Ding 1 , Yan Xu 1 , Min Hu 2 , Lidia Morawska 10 , Sergey A Grinshpun 11 , Pratim Biswas 12 , Richard C Flagan 13 , Baoli Zhu 1, 14 , Wenqing Liu 15 , Yuanhang Zhang 2
Affiliation
|
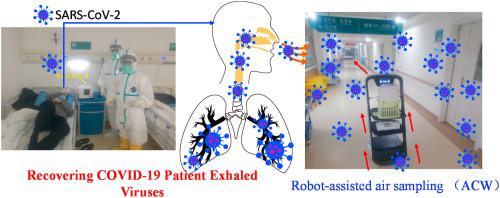
The COVID-19 pandemic has brought an unprecedented crisis to the global health sector. When discharging COVID-19 patients in accordance with throat or nasal swab protocols using reverse transcription polymerase chain reaction (RT-PCR), the potential risk of reintroducing the infection source to humans and the environment must be resolved. Here, 14 patients including 10 COVID-19 subjects were recruited; exhaled breath condensate (EBC), air samples and surface swabs were collected and analyzed for SARS-CoV-2 using reverse transcription-polymerase chain reaction (RT-PCR) in four hospitals with applied natural ventilation and disinfection practices in Wuhan. Here we discovered that 22.2% of COVID-19 patients (n = 9), who were ready for hospital discharge based on current guidelines, had SARS-CoV-2 in their exhaled breath (∼105 RNA copies/m3). Although fewer surface swabs (3.1%, n = 318) tested positive, medical equipment such as face shield frequently contacted/used by healthcare workers and the work shift floor were contaminated by SARS-CoV-2 (3–8 viruses/cm2). Three of the air samples (n = 44) including those collected using a robot-assisted sampler were detected positive by a digital PCR with a concentration level of 9–219 viruses/m3. RT-PCR diagnosis using throat swab specimens had a failure rate of more than 22% in safely discharging COVID-19 patients who were otherwise still exhaling the SARS-CoV-2 by a rate of estimated ∼1400 RNA copies per minute into the air. Direct surface contact might not represent a major transmission route, and lower positive rate of air sample (6.8%) was likely due to natural ventilation (1.6–3.3 m/s) and regular disinfection practices. While there is a critical need for strengthening hospital discharge standards in preventing re-emergence of COVID-19 spread, use of breath sample as a supplement specimen could further guard the hospital discharge to ensure the safety of the public and minimize the pandemic re-emergence risk.
中文翻译:

医院中通过呼吸、空气和表面传播的 SARS-CoV-2
COVID-19大流行给全球卫生部门带来了前所未有的危机。当使用逆转录聚合酶链反应(RT-PCR)按照咽拭子或鼻拭子方案排出COVID-19患者时,必须解决将感染源重新引入人类和环境的潜在风险。这里招募了 14 名患者,其中包括 10 名 COVID-19 受试者;在武汉四家采用自然通风和消毒措施的医院中,使用逆转录聚合酶链反应 (RT-PCR) 收集呼出气冷凝物 (EBC)、空气样本和表面拭子,并分析 SARS-CoV-2。在这里,我们发现,根据现行指南准备出院的 COVID-19 患者 (n = 9) 中,有 22.2% 的呼出气中含有 SARS-CoV-2(约 105 个 RNA 拷贝/立方米)。尽管表面拭子检测呈阳性的情况较少(3.1%,n = 318),但医护人员经常接触/使用的面罩等医疗设备以及轮班地板均受到 SARS-CoV-2 污染(3-8 个病毒/cm2)。包括使用机器人辅助采样器采集的空气样本在内的三个空气样本 (n = 44) 通过数字 PCR 检测呈阳性,浓度水平为 9-219 个病毒/立方米。使用咽拭子样本进行 RT-PCR 诊断在安全排出 COVID-19 患者方面的失败率超过 22%,否则这些患者仍在以估计每分钟约 1400 个 RNA 拷贝的速度将 SARS-CoV-2 呼出到空气中。直接表面接触可能不代表主要传播途径,空气样本阳性率较低(6.8%)可能是由于自然通风(1.6-3.3 m/s)和定期消毒措施所致。虽然迫切需要加强出院标准以防止 COVID-19 再次传播,但使用呼吸样本作为补充样本可以进一步保护出院,以确保公众的安全并最大限度地减少大流行的再次出现风险。
更新日期:2021-02-01
中文翻译:

医院中通过呼吸、空气和表面传播的 SARS-CoV-2
COVID-19大流行给全球卫生部门带来了前所未有的危机。当使用逆转录聚合酶链反应(RT-PCR)按照咽拭子或鼻拭子方案排出COVID-19患者时,必须解决将感染源重新引入人类和环境的潜在风险。这里招募了 14 名患者,其中包括 10 名 COVID-19 受试者;在武汉四家采用自然通风和消毒措施的医院中,使用逆转录聚合酶链反应 (RT-PCR) 收集呼出气冷凝物 (EBC)、空气样本和表面拭子,并分析 SARS-CoV-2。在这里,我们发现,根据现行指南准备出院的 COVID-19 患者 (n = 9) 中,有 22.2% 的呼出气中含有 SARS-CoV-2(约 105 个 RNA 拷贝/立方米)。尽管表面拭子检测呈阳性的情况较少(3.1%,n = 318),但医护人员经常接触/使用的面罩等医疗设备以及轮班地板均受到 SARS-CoV-2 污染(3-8 个病毒/cm2)。包括使用机器人辅助采样器采集的空气样本在内的三个空气样本 (n = 44) 通过数字 PCR 检测呈阳性,浓度水平为 9-219 个病毒/立方米。使用咽拭子样本进行 RT-PCR 诊断在安全排出 COVID-19 患者方面的失败率超过 22%,否则这些患者仍在以估计每分钟约 1400 个 RNA 拷贝的速度将 SARS-CoV-2 呼出到空气中。直接表面接触可能不代表主要传播途径,空气样本阳性率较低(6.8%)可能是由于自然通风(1.6-3.3 m/s)和定期消毒措施所致。虽然迫切需要加强出院标准以防止 COVID-19 再次传播,但使用呼吸样本作为补充样本可以进一步保护出院,以确保公众的安全并最大限度地减少大流行的再次出现风险。









































 京公网安备 11010802027423号
京公网安备 11010802027423号