当前位置:
X-MOL 学术
›
Microb. Biotechnol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Modulation of gut mucosal microbiota as a mechanism of probiotics-based adjunctive therapy for ulcerative colitis.
Microbial Biotechnology ( IF 4.8 ) Pub Date : 2020-09-23 , DOI: 10.1111/1751-7915.13661 Ping Chen 1 , Haiyan Xu 2 , Hai Tang 2 , Feiyan Zhao 2 , Chengcong Yang 2 , Lai-Yu Kwok 2 , Chunli Cong 1 , YanFang Wu 1 , Wenyi Zhang 2 , XiaoFeng Zhou 3 , Heping Zhang 2
Microbial Biotechnology ( IF 4.8 ) Pub Date : 2020-09-23 , DOI: 10.1111/1751-7915.13661 Ping Chen 1 , Haiyan Xu 2 , Hai Tang 2 , Feiyan Zhao 2 , Chengcong Yang 2 , Lai-Yu Kwok 2 , Chunli Cong 1 , YanFang Wu 1 , Wenyi Zhang 2 , XiaoFeng Zhou 3 , Heping Zhang 2
Affiliation
|
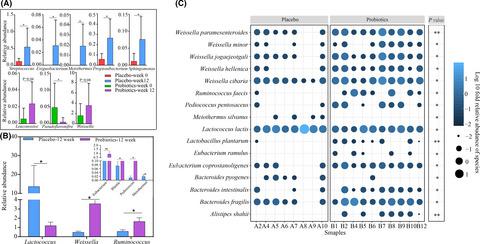
This was a pilot study aiming to evaluate the effects of probiotics as adjunctive treatment for ulcerative colitis (UC). Twenty‐five active patients with UC were assigned to the probiotic (n = 12) and placebo (n = 13) groups. The probiotic group received mesalazine (60 mg kg−1 day−1) and oral probiotics (containing Lactobacillus casei Zhang, Lactobacillus plantarum P‐8 and Bifidobacterium animalis subsp. lactis V9) twice daily for 12 weeks, while the placebo group received the same amounts of mesalazine and placebo. The clinical outcomes were assessed. The gut mucosal microbiota was profiled by PacBio single‐molecule, real‐time (SMRT) sequencing of the full‐length 16S rRNA of biopsy samples obtained by colonoscopy. A significantly greater magnitude of reduction was observed in the UC disease activity index (UCDAI) in the probiotic group compared with the placebo group (P = 0.043), accompanying by a higher remission rate (91.67% for probiotic‐receivers versus 69.23% for placebo‐receivers, P = 0.034). The probiotics could protect from diminishing of the microbiota diversity and richness. Moreover, the gut mucosal microbiota of the probiotic‐receivers had significantly more beneficial bacteria like Eubacterium ramulus (P < 0.05), Pediococcus pentosaceus (P < 0.05), Bacteroides fragilis (P = 0.02) and Weissella cibaria (P = 0.04). Additionally, the relative abundances of the beneficial bacteria correlated significantly but negatively with the UCDAI score, suggesting that the probiotics might alleviate UC symptoms by modulating the gut mucosal microbiota. Our research has provided new insights into the mechanism of symptom alleviation in UC by applying probiotic‐based adjunctive treatment.
中文翻译:

调节肠粘膜微生物群作为基于益生菌的溃疡性结肠炎辅助治疗的机制。
这是一项初步研究,旨在评估益生菌作为溃疡性结肠炎 (UC) 辅助治疗的效果。 25 名活动性 UC 患者被分配到益生菌组 ( n = 12) 和安慰剂组 ( n = 13)。益生菌组每天两次服用美沙拉嗪(60 mg kg -1天-1 )和口服益生菌(含有干酪乳杆菌、植物乳杆菌P-8 和动物双歧杆菌乳亚种 V9),持续 12 周,而安慰剂组接受相同的治疗一定量的美沙拉秦和安慰剂。评估临床结果。通过对结肠镜检查获得的活检样本的全长 16S rRNA 进行 PacBio 单分子实时 (SMRT) 测序,对肠道粘膜微生物群进行分析。与安慰剂组相比,益生菌组的 UC 疾病活动指数 (UCDAI) 降低幅度显着更大 ( P = 0.043),并且缓解率更高(益生菌接受组为 91.67%,安慰剂组为 69.23%) ‐接收者, P = 0.034)。益生菌可以防止微生物群多样性和丰富度的减少。此外,益生菌接受者的肠道粘膜微生物群具有显着更多的有益细菌,如枝真杆菌( P < 0.05)、戊糖片球菌( P < 0.05)、脆弱拟杆菌( P = 0.02)和Weissell cibaria ( P = 0.04)。 此外,有益细菌的相对丰度与 UCDAI 评分显着但负相关,表明益生菌可能通过调节肠道粘膜微生物群来缓解 UC 症状。我们的研究为通过应用基于益生菌的辅助治疗缓解 UC 症状的机制提供了新的见解。
更新日期:2020-10-05
中文翻译:

调节肠粘膜微生物群作为基于益生菌的溃疡性结肠炎辅助治疗的机制。
这是一项初步研究,旨在评估益生菌作为溃疡性结肠炎 (UC) 辅助治疗的效果。 25 名活动性 UC 患者被分配到益生菌组 ( n = 12) 和安慰剂组 ( n = 13)。益生菌组每天两次服用美沙拉嗪(60 mg kg -1天-1 )和口服益生菌(含有干酪乳杆菌、植物乳杆菌P-8 和动物双歧杆菌乳亚种 V9),持续 12 周,而安慰剂组接受相同的治疗一定量的美沙拉秦和安慰剂。评估临床结果。通过对结肠镜检查获得的活检样本的全长 16S rRNA 进行 PacBio 单分子实时 (SMRT) 测序,对肠道粘膜微生物群进行分析。与安慰剂组相比,益生菌组的 UC 疾病活动指数 (UCDAI) 降低幅度显着更大 ( P = 0.043),并且缓解率更高(益生菌接受组为 91.67%,安慰剂组为 69.23%) ‐接收者, P = 0.034)。益生菌可以防止微生物群多样性和丰富度的减少。此外,益生菌接受者的肠道粘膜微生物群具有显着更多的有益细菌,如枝真杆菌( P < 0.05)、戊糖片球菌( P < 0.05)、脆弱拟杆菌( P = 0.02)和Weissell cibaria ( P = 0.04)。 此外,有益细菌的相对丰度与 UCDAI 评分显着但负相关,表明益生菌可能通过调节肠道粘膜微生物群来缓解 UC 症状。我们的研究为通过应用基于益生菌的辅助治疗缓解 UC 症状的机制提供了新的见解。









































 京公网安备 11010802027423号
京公网安备 11010802027423号