JACC: Heart Failure ( IF 10.3 ) Pub Date : 2020-08-12 , DOI: 10.1016/j.jchf.2020.05.013 Stephen J Greene 1 , Taylor S Triana 2 , Raluca Ionescu-Ittu 3 , Rebecca M Burne 3 , Annie Guérin 3 , Maria Borentain 4 , Paul D Kessler 4 , Aylin Tugcu 4 , Mary M DeSouza 4 , G Michael Felker 1 , Lei Chen 4
|
Objectives
This study sought to characterize in-hospital treatment patterns and associated patient outcomes among patients hospitalized for heart failure (HF) in U.S. clinical practice.
Background
Hospitalizations for HF are common and associated with poor patient outcomes. Real-world patterns of in-hospital treatment, including diuretic therapy, in contemporary U.S. practice are unknown.
Methods
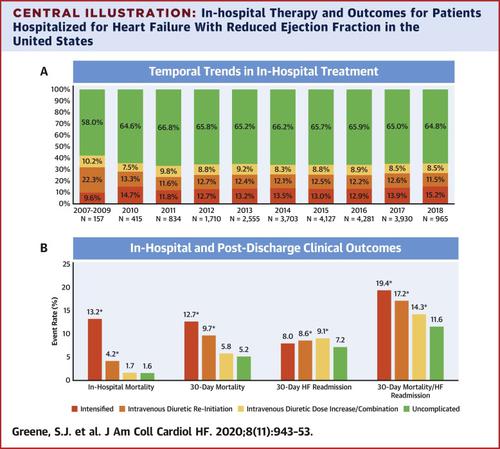
Using Optum de-identified Electronic Health Record data from 2007 through 2018, patients hospitalized for a primary diagnosis of HF (ejection fraction ≤40%) and who were hemodynamically stable at admission, without concurrent acute coronary syndrome or end-stage renal disease, and treated with intravenous (IV) diuretic agents within 48 h of admission were identified. Patients were categorized into 1 of 4 mutually exclusive hierarchical treatment groups defined by complexity of treatment during hospitalization (intensified treatment with mechanical support or IV vasoactive therapy, IV diuretic therapy reinitiated after discontinuation for ≥1 day without intensified treatment, IV diuretic dose increase/combination diuretic treatment without intensified treatment or IV diuretic reinitiation, or uncomplicated).
Results
Of 22,677 patients hospitalized for HF with reduced ejection fraction (HFrEF), 66% had uncomplicated hospitalizations without escalation of treatment beyond initial IV diuretic therapy. Among 7,809 remaining patients, the highest level of therapy received was IV diuretic dose increase/combination diuretic treatment in 25%, IV diuretic reinitiation in 36%, and intensified therapy in 39%. Overall, 19% of all patients had reinitiation of IV diuretic agents (26% of such patients had multiple instances), 12% were simultaneously treated with multiple diuretics, and 61% were transitioned to oral diuretic agents before discharge. Compared with uncomplicated treatment, IV diuretic reinitiation and intensified treatment were associated with significantly longer median length of stay (uncomplicated: 4 days; IV diuretic reinitiation: 8 days; intensified: 10 days) and higher rates of in-hospital (uncomplicated: 1.6%; IV diuretic reinitiation: 4.2%; intensified: 13.2%) and 30-day post-discharge mortality (uncomplicated: 5.2%; IV diuretic reinitiation: 9.7%; intensified: 12.7%).
Conclusions
In this contemporary real-world population of U.S. patients hospitalized for HFrEF, one-third of patients had in-hospital treatment escalated beyond initial IV diuretic therapy. These more complex treatment patterns were associated with highly variable patterns of diuretic use, longer hospital lengths of stay, and higher mortality. Standardized and evidence-based approaches are needed to improve the efficiency and effectiveness of in-hospital HFrEF care.
中文翻译:

在美国,心力衰竭的住院治疗与射血分数降低有关。
目标
这项研究试图在美国临床实践中表征因心力衰竭(HF)住院的患者的住院治疗模式和相关患者结局。
背景
心力衰竭的住院很普遍,并且与患者预后差有关。在美国当代实践中,包括利尿剂在内的医院内治疗的实际模式尚不清楚。
方法
使用2007年至2018年间使用Optum取消身份识别的电子健康记录数据,住院进行HF初次诊断(射血分数≤40%)且入院时血流动力学稳定,无并发急性冠脉综合征或终末期肾病的患者,以及确认在入院后48小时内用静脉利尿剂治疗。根据住院期间的治疗复杂性将患者分为4种互斥的分层治疗组中的1组(机械支持或IV血管活性治疗的强化治疗,停药≥1天而未接受强化治疗的情况下重新开始IV利尿治疗,IV利尿剂剂量增加/联合使用)利尿剂治疗,而无需加强治疗或静脉利尿剂重新开始或不复杂)。
结果
在22677例因射血分数降低(HFrEF)而住院的HF患者中,有66%的患者住院简单,并且未进行超出初始静脉利尿剂治疗的治疗。在剩余的7,809名患者中,接受的最高治疗水平是静脉利尿剂剂量增加/联合利尿剂治疗(25%),静脉利尿剂重新开始(36%)和强化治疗(39%)。总体而言,所有患者中有19%的患者重新使用了静脉利尿剂(其中26%的患者曾多次复吸),同时有12%的患者同时接受了多种利尿剂治疗,而61%的患者在出院前已改用口服利尿剂。与单纯治疗相比,静脉利尿剂重新开始和强化治疗与中位住院时间明显更长有关(单纯:4天;静脉利尿重新开始:8天;强化:
结论
在接受HFrEF住院治疗的美国当代患者中,有三分之一的患者住院治疗已超出了最初的静脉利尿剂治疗。这些更复杂的治疗方式与利尿剂使用方式变化很大,住院时间更长和死亡率更高有关。需要采用标准化且循证的方法来提高院内HFrEF护理的效率和有效性。











































 京公网安备 11010802027423号
京公网安备 11010802027423号