JACC: Heart Failure ( IF 10.3 ) Pub Date : 2020-08-12 , DOI: 10.1016/j.jchf.2020.04.019 Marilyne Jarjour 1 , Christine Henri 1 , Simon de Denus 1 , Annik Fortier 2 , Nadia Bouabdallaoui 1 , Anil Nigam 1 , Eileen O'Meara 1 , Charaf Ahnadi 3 , Michel White 1 , Patrick Garceau 1 , Normand Racine 1 , Marie-Claude Parent 1 , Mark Liszkowski 1 , Geneviève Giraldeau 1 , Jean-Lucien Rouleau 1 , Anique Ducharme 1
|
Objectives
This study evaluated the impact of clinical and physiological factors limiting treatment optimization toward recommended medical therapy in heart failure (HF).
Background
Although guidelines aim to assist physicians in prescribing evidence-based therapies and to improve outcomes of patients with HF and reduced ejection fraction (HFrEF), gaps in clinical care persist.
Methods
Medical records of all patients with HFrEF followed for at least 6 months at the authors’ HF clinic (n = 511) allowed for drug optimization and were reviewed regarding the prescription rates of recommended pharmacological agents and devices (implantable cardioverter-defibrillator [ICD] or cardiac resynchronization therapy [CRT]). Then, an algorithm integrating clinical (New York Heart Association [NYHA] functional class, heart rate, blood pressure and biologic parameters (creatinine, serum potassium) based on the inclusion/exclusion criteria of landmark trials guiding these recommendations) was applied for each agent and device to identify potential explanations for treatment gaps.
Results
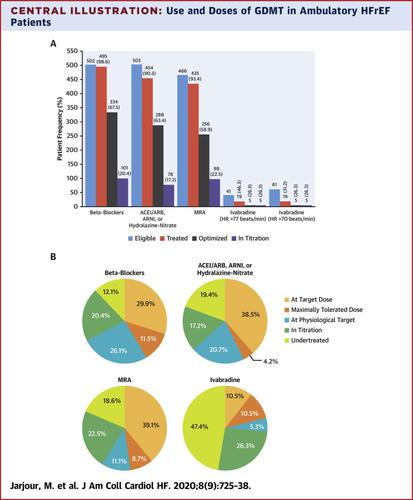
Gross prescription rates were high for beta-blockers (98.6%), mineralocorticoid receptor antagonist (MRA) (93.4%), vasodilators (90.3%), ICDs (75.1%), and CRT (82.1%) among those eligible, except for ivabradine (46.3%, n = 41). However, achievement of target physiological doses was lower (beta-blockers, 67.5%; MRA, 58.9%; and vasodilators, 63.4%), and one-fifth of patient dosages were still being up-titrated. Suboptimal doses were associated with older age (odds ratio [OR]: 1.221; p < 0.0001) and history of stroke or transient ischemic attack (TIA) (no vs. yes, OR: 0.264; p = 0.0336).
Conclusions
Gaps in adherence to guidelines exist in specialized HF setting and are mostly explained by limiting physiological factors rather than inertia. Older age and history of stroke/TIA, potential markers of frailty, are associated with suboptimal doses of guideline-directed medical therapy, suggesting that an individualized rather than a “one-size-fits-all” approach may be required.
中文翻译:

遵守心力衰竭指南的护理差距:临床惯性或生理限制?
目标
本研究评估了限制治疗优化的临床和生理因素对心力衰竭 (HF) 推荐药物治疗的影响。
背景
尽管指南旨在协助医生开具循证疗法并改善心衰和射血分数降低 (HFrEF) 患者的预后,但临床护理方面的差距仍然存在。
方法
在作者的 HF 诊所(n = 511)随访至少 6 个月的所有 HFrEF 患者的医疗记录允许进行药物优化,并就推荐的药物制剂和设备(植入式心律转复除颤器 [ICD] 或心脏再同步治疗 [CRT])。然后,将临床(纽约心脏协会 [NYHA] 功能分类、心率、血压和生物参数(肌酐、血清钾)基于指导这些建议的里程碑式试验的纳入/排除标准)应用于每种药物和设备来确定治疗差距的潜在解释。
结果
除伊伐布雷定外,β受体阻滞剂 (98.6%)、盐皮质激素受体拮抗剂 (MRA) (93.4%)、血管扩张剂 (90.3%)、ICD (75.1%) 和 CRT (82.1%) 的总处方率较高(46.3%,n = 41)。然而,目标生理剂量的实现较低(β 受体阻滞剂,67.5%;MRA,58.9%;血管扩张剂,63.4%),并且五分之一的患者剂量仍在滴定。次优剂量与年龄较大(比值比 [OR]:1.221;p < 0.0001)和中风史或短暂性脑缺血发作 (TIA) 相关(否与是,OR:0.264;p = 0.0336)。
结论
遵循指南的差距存在于专门的 HF 环境中,主要是通过限制生理因素而不是惯性来解释的。年龄较大和中风/TIA 病史是虚弱的潜在标志,与指南指导的药物治疗剂量不理想有关,这表明可能需要个体化而不是“一刀切”的方法。











































 京公网安备 11010802027423号
京公网安备 11010802027423号