JACC: Heart Failure ( IF 10.3 ) Pub Date : 2020-08-12 , DOI: 10.1016/j.jchf.2020.06.009 Madeline R Sterling 1 , Lisa M Kern 1 , Monika M Safford 1 , Christine D Jones 2 , Penny H Feldman 3 , Gregg C Fonarow 4 , Shubin Sheng 5 , Roland A Matsouaka 6 , Adam D DeVore 6 , Barbara Lytle 6 , Haolin Xu 6 , Larry A Allen 2 , Anita Deswal 7 , Clyde W Yancy 8 , Nancy M Albert 9
|
Objectives
This study compared the characteristics of Medicare beneficiaries who were hospitalized for heart failure (HF) and then discharged home who received home health care (HHC) to the characteristics of those who did not, and examined associations among HHC and readmission and mortality rates.
Background
After hospitalization for HF, some patients receive HHC. However, the use of HHC over time, the factors associated with its use, and the post-discharge outcomes after receiving it are not well studied.
Methods
This study used Get With The Guidelines-HF data, merged with Medicare fee-for-service claims. Propensity score matching and Cox proportional hazards models were used to evaluate the associations between HHC and post-discharge outcomes.
Results
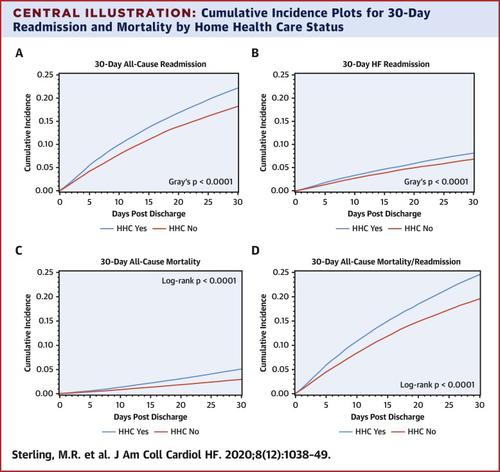
From 2005 to 2015, 95,531 patients were admitted for HF, and 32,697 (34.2%) received HHC after discharge. The rate of HHC increased over time from 31.4% to 36.1% (p < 0.001). HHC recipients were older, more likely to be female, and had more comorbidities. HHC was associated with a higher risk of all-cause 30-day readmission (hazard ratio [HR]: 1.25; 95% confidence interval [CI]: 1.20 to 1.30), HF-specific 30-day readmission (HR: 1.20; 95% CI: 1.13 to 1.28), all-cause 90-day readmission (HR: 1.23; 95% CI: 1.19 to 1.26), HF-specific 90-day readmission (HR: 1.16; 95% CI: 1.11 to 1.22), and all-cause 30-and 90-day mortality, respectively (HR: 1.70; 95% CI: 1.56 to 1.86) and HR: 1.49; 95% CI: 1.41 to 1.57) compared to those who did not receive HHC.
Conclusions
Use of HHC after HF hospitalization increased among Medicare beneficiaries. HHC recipients were older and sicker than non-HHC recipients. Although HHC was associated with a higher risk of readmissions and mortality, this finding should be interpreted cautiously, given the presence of unmeasured variables that could affect receipt of HHC. Research is needed to determine whether the results reflect appropriate health care use.
中文翻译:

心力衰竭住院后的家庭保健使用和出院后结果。
目标
本研究比较了因心力衰竭 (HF) 住院然后出院并接受家庭医疗保健 (HHC) 的医疗保险受益人的特征与未接受家庭医疗保健 (HHC) 的人的特征,并检查了 HHC 与再入院率和死亡率之间的关联。
背景
在因 HF 住院后,一些患者接受 HHC。然而,HHC 的长期使用、与其使用相关的因素以及接受 HHC 后的出院后结果尚未得到很好的研究。
方法
本研究使用 Get With The Guidelines-HF 数据,并与 Medicare 按服务收费索赔合并。倾向评分匹配和 Cox 比例风险模型用于评估 HHC 与出院后结果之间的关联。
结果
从 2005 年到 2015 年,95,531 名患者因 HF 入院,32,697 人(34.2%)在出院后接受 HHC。HHC 的发生率随时间从 31.4% 增加到 36.1% (p < 0.001)。HHC 接受者年龄较大,更有可能是女性,并且有更多的合并症。HHC 与更高的全因 30 天再入院风险相关(风险比 [HR]:1.25;95% 置信区间 [CI]:1.20 至 1.30)、HF 特异性 30 天再入院(HR:1.20;95 % CI:1.13 至 1.28),全因 90 天再入院(HR:1.23;95% CI:1.19 至 1.26),HF 特异性 90 天再入院(HR:1.16;95% CI:1.11 至 1.22),和全因 30 天和 90 天死亡率分别为(HR:1.70;95% CI:1.56 至 1.86)和 HR:1.49;95% CI:1.41 到 1.57)与未接受 HHC 的人相比。
结论
在医疗保险受益人中,HF 住院后 HHC 的使用增加。HHC 接受者比非 HHC 接受者年龄更大、病情更重。尽管 HHC 与更高的再入院和死亡风险相关,但鉴于存在可能影响 HHC 接受的未测量变量,应谨慎解释这一发现。需要进行研究以确定结果是否反映了适当的医疗保健用途。









































 京公网安备 11010802027423号
京公网安备 11010802027423号