当前位置:
X-MOL 学术
›
Adv. Healthcare Mater.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Sustained Release of TPCA-1 from Silk Fibroin Hydrogels Preserves Keratocyte Phenotype and Promotes Corneal Regeneration by Inhibiting Interleukin-1β Signaling.
Advanced Healthcare Materials ( IF 10.0 ) Pub Date : 2020-08-02 , DOI: 10.1002/adhm.202000591 Wei Zhang 1, 2, 3 , Jialin Chen 1, 2, 3 , Mingli Qu 4 , Ludvig J Backman 2 , Aini Zhang 1 , Haoyang Liu 1 , Xiaoping Zhang 5 , Qingjun Zhou 4 , Patrik Danielson 2, 6
Advanced Healthcare Materials ( IF 10.0 ) Pub Date : 2020-08-02 , DOI: 10.1002/adhm.202000591 Wei Zhang 1, 2, 3 , Jialin Chen 1, 2, 3 , Mingli Qu 4 , Ludvig J Backman 2 , Aini Zhang 1 , Haoyang Liu 1 , Xiaoping Zhang 5 , Qingjun Zhou 4 , Patrik Danielson 2, 6
Affiliation
|
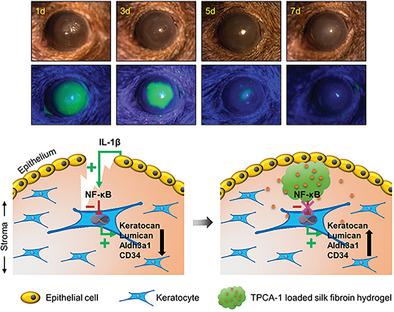
Corneal injury due to ocular trauma or infection is one of the most challenging vision impairing pathologies that exists. Many studies focus on the pro‐inflammatory and pro‐angiogenic effects of interleukin‐1β (IL‐1β) on corneal wound healing. However, the effect of IL‐1β on keratocyte phenotype and corneal repair, as well as the underlying mechanisms, is not clear. This study reports, for the first time, that IL‐1β induces phenotype changes of keratocytes in vitro, by significantly down‐regulating the gene and protein expression levels of keratocyte markers (Keratocan, Lumican, Aldh3a1 and CD34). Furthermore, it is found that the NF‐κB pathway is involved in the IL‐1β‐induced changes of keratocyte phenotype, and that the selective IKKβ inhibitor TPCA‐1, which inhibits NF‐κB, can preserve keratocyte phenotype under IL‐1β simulated pathological conditions in vitro. By using a murine model of corneal injury, it is shown that sustained release of TPCA‐1 from degradable silk fibroin hydrogels accelerates corneal wound healing, improves corneal transparency, enhances the expression of keratocyte markers, and supports the regeneration of well‐organized epithelium and stroma. These findings provide insights not only into the pathophysiological mechanisms of corneal wound healing, but also into the potential development of new treatments for patients with corneal injuries.
中文翻译:

TPCA-1从丝素蛋白水凝胶的持续释放通过抑制白介素-1β信号传导保留了角膜细胞表型并促进了角膜再生。
由眼外伤或感染引起的角膜损伤是存在的最具挑战性的视力损害病理学之一。许多研究集中于白细胞介素-1的促炎症和促血管生成作用β(IL-1 β的角膜伤口愈合)。但是,尚不清楚IL- 1β对角膜细胞表型和角膜修复的影响以及潜在的机制。该研究报告,对于第一次,IL-1 β的角膜细胞体外诱导的表型变化,通过显著下调角膜标记(Keratocan,基膜聚糖,ALDH3A1和CD34)的基因和蛋白表达水平。此外,还发现,NF- κ乙途径参与在IL-1 β角膜表型诱导的变化,并且所述选择性IKK β抑制剂TPCA-1,其抑制NF- κ B,可以保留角膜下IL-1表型的β模拟体外病理状况。通过使用鼠类角膜损伤模型,可降解的丝素蛋白水凝胶持续释放TPCA-1可以加速角膜伤口愈合,改善角膜透明性,增强角膜细胞标记物的表达,并支持组织良好的上皮细胞的再生。基质。这些发现不仅为角膜伤口愈合的病理生理机制提供了见识,而且还为角膜损伤患者的新疗法的潜在开发提供了见识。
更新日期:2020-09-10
中文翻译:

TPCA-1从丝素蛋白水凝胶的持续释放通过抑制白介素-1β信号传导保留了角膜细胞表型并促进了角膜再生。
由眼外伤或感染引起的角膜损伤是存在的最具挑战性的视力损害病理学之一。许多研究集中于白细胞介素-1的促炎症和促血管生成作用β(IL-1 β的角膜伤口愈合)。但是,尚不清楚IL- 1β对角膜细胞表型和角膜修复的影响以及潜在的机制。该研究报告,对于第一次,IL-1 β的角膜细胞体外诱导的表型变化,通过显著下调角膜标记(Keratocan,基膜聚糖,ALDH3A1和CD34)的基因和蛋白表达水平。此外,还发现,NF- κ乙途径参与在IL-1 β角膜表型诱导的变化,并且所述选择性IKK β抑制剂TPCA-1,其抑制NF- κ B,可以保留角膜下IL-1表型的β模拟体外病理状况。通过使用鼠类角膜损伤模型,可降解的丝素蛋白水凝胶持续释放TPCA-1可以加速角膜伤口愈合,改善角膜透明性,增强角膜细胞标记物的表达,并支持组织良好的上皮细胞的再生。基质。这些发现不仅为角膜伤口愈合的病理生理机制提供了见识,而且还为角膜损伤患者的新疗法的潜在开发提供了见识。











































 京公网安备 11010802027423号
京公网安备 11010802027423号